Current international diagnostic criteria for multiple sclerosis (MS) do not include the optic nerve as an imaging lesion site, despite the high prevalence of acute optic neuritis (ON) among early MS patients. Since the latest evaluation of these criteria in 2017, neuro-ophthalmologists Laura J. Balcer, MD, and Steven L. Galetta, MD, have been adding to the evidence for incorporation of the optic nerve into MS diagnostics.
“About 25 percent of MS patients have ON as their first manifestation. However, research that patients who present with spinal cord or brainstem lesions on MRI typically progress to MS, left people with ON at a disadvantage. Their lesions in the optic nerve weren’t counted,” Dr. Galetta says.
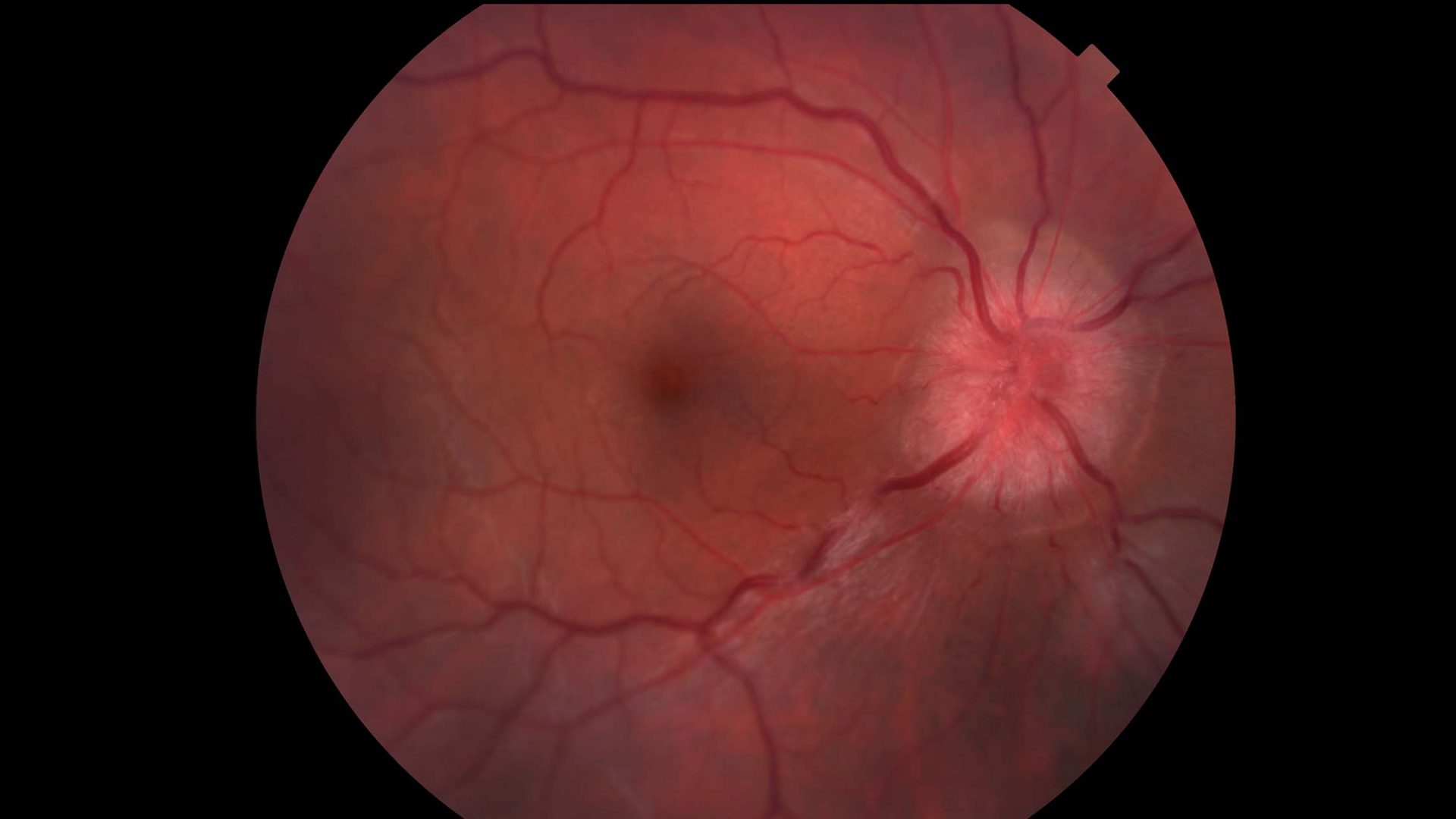
Studies have suggested that inter-eye differences in retinal nerve fiber layer thickness, as measured by spectral-domain optical coherence tomography (SD-OCT), optimize identification of people with a history of ON.
“Imaging the optic nerve with OCT is more sensitive for indicating there’s been a demyelinating event,” Dr. Balcer says. “In a younger person, there are a limited number of entities besides MS that could cause thinning of the axonal layer.”
“About 25 percent of MS patients have ON as their first manifestation.”
Steven L. Galetta, MD
Building the Case for Inclusion
In a foundational study in 2017, Dr. Balcer and colleagues established the validity of low-contrast letter acuity (LCLA) as a visual performance outcome measure for MS over high-contrast visual acuity, which has been used for decades. Deficits in LCLA and vision-specific quality of life are found many years after an episode of acute ON, even when high-contrast visual acuity has recovered.
Several further studies have aided in determining optimal thresholds for inter-eye differences in retinal layer thickness that are most predictive of a unilateral optic nerve lesion.
In a single-center analysis comparing healthy volunteers to people with MS, and then in a multicenter study with the International MS Visual System Consortium, the researchers confirmed inter-eye differences of 5μm for the peripapillary retinal nerve fiber layer (pRNFL) and 4μm for the macular ganglion cell inner plexiform layer (GCIPL) as robust thresholds.
“Low-contrast acuity was shown to detect the subtle deficits. Then, OCT came along to validate that. It turned out to be an even stronger structure/function coordination than we had thought,” Dr. Balcer says.
Evaluating Long-Term Outcomes
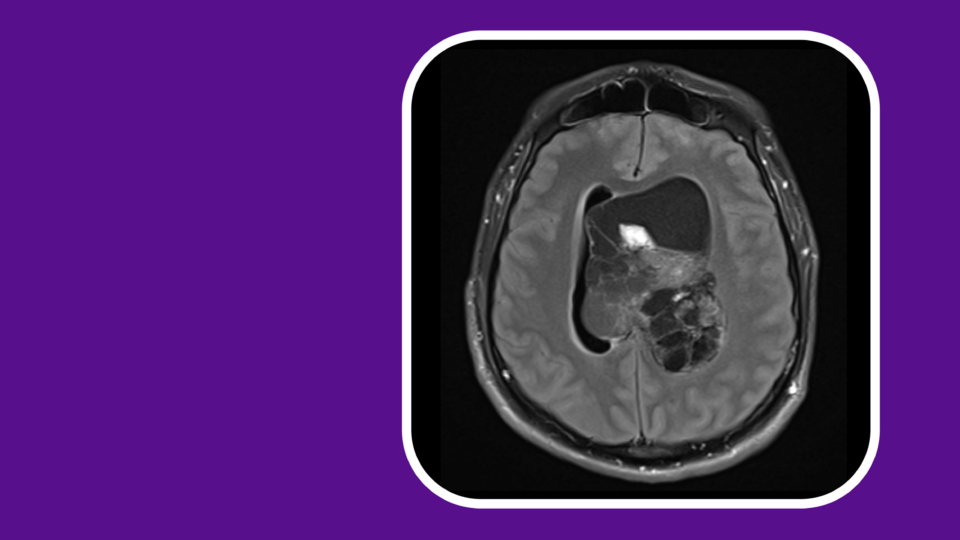
The next step was to demonstrate that early diagnosis of ON and initiation of MS treatment would slow disease progression. The researchers used a cohort from MSBase, an international online registry containing about 80,000 patient records.
“The MSBase study is a longer study – 5 years – and people tended not to exit once they were in it,” Dr. Galetta notes. “We were able to look at disability, both visually and that initial treatment trials of the clinically isolated syndrome didn’t include.”
In the MSBase cohort, early treatment after ON diagnosis was associated with better long-term visual and neurological outcomes compared to no treatment. The results support early treatment for patients presenting with ON as the first manifestation of MS.
“Low-contrast acuity was shown to detect the subtle deficits. Then, OCT came along to validate that.”
Laura J. Balcer, MD
Assessing Diagnostic Accuracy
In new research soon to be published, a team including Dr. Balcer, Dr. Galetta and Rachel Kenney, PhD, a former NYU Langone Health neuro-ophthalmology fellow, demonstrate that a composite score incorporating visual function tests such as LCLA, combined with SD-OCT measurements, improves the ability to identify patients with MS. The research team includes colleagues in the Advanced Ophthalmic Imaging Lab and from several partnering institutions.
The researchers measured pRNFL and GCIPL thicknesses on SD-OCT devices and developed a composite score, combining OCT and other visual measures. They compared this score with individual measurements to determine the best model, and used support vector machine analysis to confirm that the model improved the diagnostic capability of OCT.
The study provides class III evidence that SD-OCT can accurately distinguish people with MS from others and those with a history of unilateral ON. Combined with the MSBase evidence for improved outcomes, the team is hoping the findings are enough to get ON added to the MS criteria in the next evaluation.
“Vision has always been last to the table. We’ve had to prove everything beyond a reasonable doubt. It’s been really gratifying to be able to present such strong evidence,” Dr. Galetta says.