A recent study found that patients on certain disease-modifying therapies (DMTs) for multiple sclerosis (MS) had markedly impaired adaptive immune responses to SARS-CoV-2 infection, although immune responses did not correlate with COVID-19 clinical severity.
Lead researcher Ilya Kister, MD, a professor of neurology, says the team was surprised by the findings.
“Understanding the impact of DMTs on the immune response to SARS-CoV-2 is critical for counseling patients with MS about COVID-19 risks and determining whether a patient on a particular DMT is likely to derive a similar degree of protective immunity as healthy individuals,” Dr. Kister says.
Responses After Natural Infection
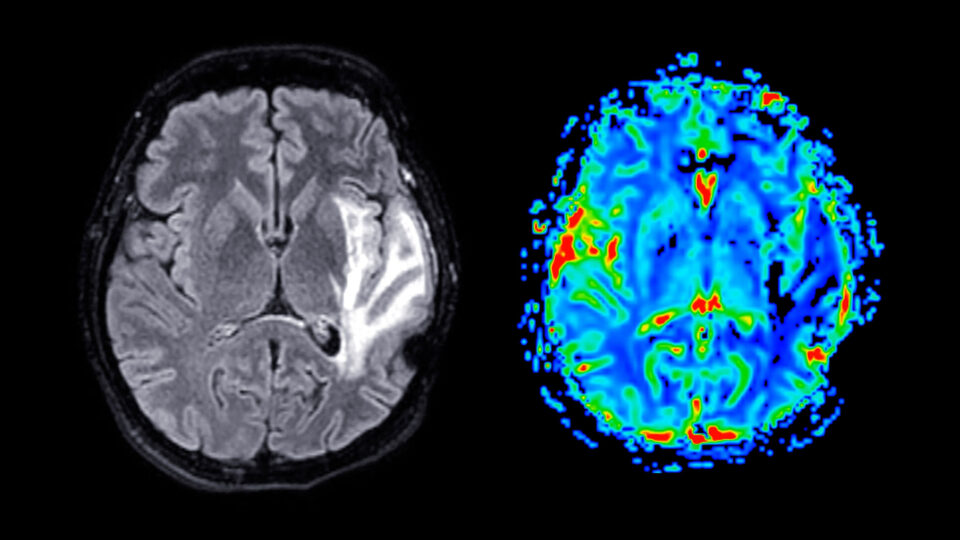
MS is treated with several therapies that may impair immune responses to SARS-CoV-2 infection. The widely used anti-CD20 (aCD20) therapies have been associated with reduced antibody titers following infection, potentially due to depletion of peripheral B cells that would otherwise be available for recruitment into germinal centers for antigen-mediated activation and clonal expansion.
“T cell responses following natural infection in aCD20-treated patients have received less attention, but are an active area of investigation,” Dr. Kister says.
“Our relatively young and otherwise healthy MS patients on various DMTs generally had favorable clinical course despite markedly impaired adaptive immune responses associated with some of the DMTs, including aCD20 therapies and S1P receptor modulators”
Ilya Kister, MD
Research Design and Findings
Between January and July 2021, 389 patients with clinician-diagnosed MS aged 18 to 60 years were tested for anti-nucleocapsid and anti-spike receptor-binding domain (RBD) antibodies. Antibody responses to spike protein, RBD and N-terminal domain (NTD), and T cell responses to SARS-CoV-2 spike protein were also tested using a variety of assays.
The mean age of study participants was 40.3 years; 74 percent were female and 62 percent were non-white. The most common DMTs were ocrelizumab (40 percent), natalizumab (17 percent), and sphingosine 1-phosphate (S1P) receptor modulators (12 percent).
After testing, 177 patients (46 percent) had laboratory-confirmed SARS-CoV-2 infection, including 130 symptomatic cases and 47 asymptomatic cases. Among the participants, COVID-19 clinical course was mild overall, with only 9 patients (7 percent) hospitalized–these results did not differ across DMTs.
Antibody responses were markedly attenuated in patients treated with ocrelizumab compared to other groups. T cell responses were significantly decreased in patients treated with S1P receptor modulators and increased in patients treated with natalizumab. Cellular and humoral responses were moderately correlated for patients treated with ocrelizumab and for patients treated with non-OCR DMTs.
Neither clinical nor immunologic outcomes differed by race/ethnicity.
Differences in DMTs
“Our relatively young and otherwise healthy MS patients on various DMTs generally had favorable clinical course despite markedly impaired adaptive immune responses associated with some of the DMTs, including aCD20 therapies and S1P receptor modulators,” Dr. Kister says. “It is also reassuring that patients whose B cells were depleted with therapy still had similarly robust T cell memory to infection as did untreated patients.”
Based on these results, Dr. Kister and his team are conducting more in-depth studies to better understand the humoral–cellular dissociation in aCD20-treated patients, and to identify predictors of immune response in patients on different DMTs.