A current challenge to understanding the pathophysiology and progression of Parkinson’s disease (PD) is identifying and validating markers for the preclinical and prodromal stages, says Giulietta M. Riboldi, MD, PhD, a research assistant professor of neurology at NYU Langone Health.
To that end, NYU Langone researchers have joined a landmark global study aimed at identifying markers of disease progression to reduce PD disability. The Parkinson’s Progression Markers Initiative (PPMI)—a groundreaking observational study across nearly 50 international sites and sponsored by The Michael J. Fox Foundation—is investigating the development of clinical features, digital outcomes, and biomarkers of PD progression in patients with manifest PD, patients with prodromal symptoms, and healthy control volunteers.
“A systematic collection of data and biosamples from patients with Parkinson’s disease at different centers around the world represents a unique platform for new research discoveries and result validation in the field,” Dr. Riboldi says.
A Transformative Study
Since its inception in 2010, the PPMI study has become a cornerstone of PD research and continues to advance new treatments. Analyses from its dataset and biosample library have deepened understanding of PD and informed the design of dozens of therapeutic trials.
With the goal of providing a more detailed and nuanced inquiry into PD development, The Michael J. Fox Foundation announced an expansion of PPMI to increase the size and diversity of enrollment cohorts. The expansion has potential downstream applications including earlier detection of those at risk, and the development of innovative new tests, treatments, and technologies.
“These markers could lead to earlier, faster diagnosis, and the development of therapies to slow, stop, or prevent the disease.”
Giulietta M. Riboldi, MD, PhD
“Each PPMI volunteer contributes to the effort toward markers that are unique to people with Parkinson’s disease or who are at risk of Parkinson’s disease,” says Dr. Riboldi. “These markers could lead to earlier, faster diagnosis, and the development of therapies to slow, stop, or prevent the disease.”
Prodromal Parkinson’s Disease and REM Sleep Behavior Disorder
Prodromal symptoms of PD are non-motor, and idiopathic REM sleep behavior disorder (RBD) is a well-established risk factor for neurodegenerative disease, with approximately 40 to 65 percent of patients with RBD also being diagnosed with a synuclein-related disorder during their lifetime.
Research efforts are underway to find a treatment for RBD. Nonetheless, with no preventive agent for PD, recruiting volunteers with prodromal PD who don’t exhibit motor symptoms requires large-scale innovative screening and recruiting efforts.
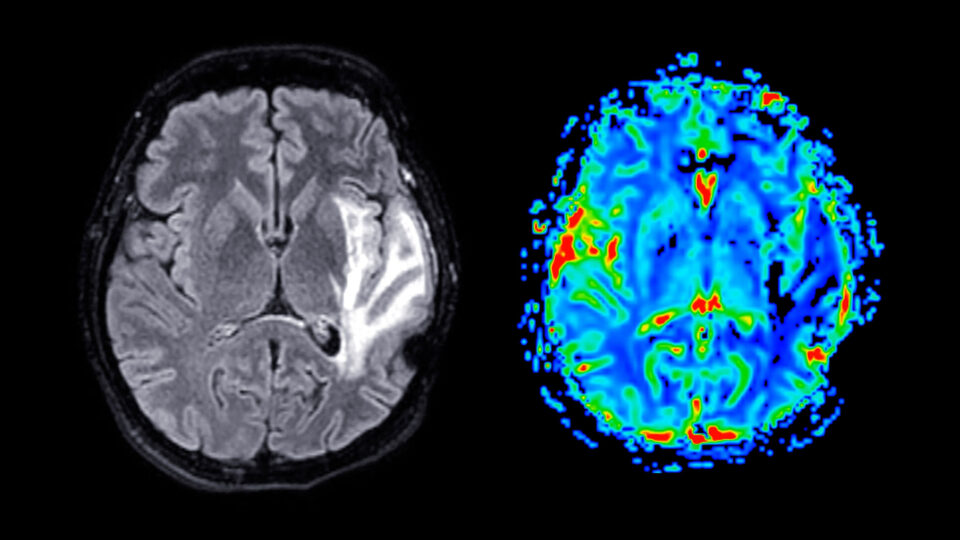
“When the motor symptoms of Parkinson’s disease manifest, the majority of the dopaminergic cells in the brain are lost,” Dr. Riboldi says. “Studying early biological changes in prodromal stages of PD can help to clarify triggering mechanisms of the disorder and identify biomarkers for early intervention.”
Although significant challenges to accrual remain, efforts are now underway at NYU Langone and collaborating institutions to recruit participants with idiopathic RBD for the study. Since idiopathic RBD is the strongest predictor of future development of α-synucleinopathies, it could be used as a model to understand the clinical and molecular evolution of the preclinical/prodromal phase of pathological α-synuclein—with the ultimate goal of initiating disease prevention studies in the prodromal phase.
PPMI’s Ambitious Expansion
The updated PPMI clinical study protocol has set a target enrollment of approximately 4,000 participants across the nearly 50 sites worldwide. Study participants are mainly identified through a stage risk paradigm using a custom-built remote platform called PPMI Online.
In addition to identifying and further characterizing biomarkers, the researchers anticipate that the updated findings may inform further studies investigating PD therapeutics including clinical trials targeting synuclein, leucine-rich repeat kinase 2 (LRRK2), glucocerebrosidase (GBA), and others.
“We hope that this effort will help identify reliable biomarkers for improving the diagnosis of PD and the development of effective disease-modifying treatments,” Dr. Riboldi explains.
These efforts complement ongoing work at NYU Langone’s Dysautonomia Center and the Parekh Center for Interdiscipinary Neurology, which are conducting basic science and clinical research that can help to illuminate the common mechanisms underlying neurodegenerative disorders.