Skeletal maintenance and healing rely heavily on stem cells to replace tissue lost to injury, disease, or wear and tear. Preserving this readiness requires skeletal stem cells to be continually renewed by cell division and kept in an immature, uncommitted state, the underlying mechanisms of which remain poorly understood. A subsequent differentiation process can then yield the bone tissue’s major cellular lineages.
Skeletal stem cells become depleted with age, however, resulting in weaker bones that are more susceptible to fracture and less adept at efficient repair and regeneration. If directed to remain in greater numbers, conversely, they might provide a rich source of replacements for lost cells or a promising therapeutic target for rejuvenating aging bones.
“Our data revealed a previously unknown function for Hox genes as essential location-specific regulators of stem cell maturity in adulthood, with short-term local increases in their expression able to drive healing.”
Philipp Leucht, MD, PhD
In a new study published in the journal Development, a group of researchers at NYU Langone Health discovered that this maintenance role in adulthood may be spearheaded by the same family of Hox (or homeobox) genes that are better known for directing bone formation during embryonic development.
A Newly Discovered Role in Adult Bone Maintenance
In mice and humans, 39 Hox genes act as site-specific transcriptional factors to guide immature stem cells in different regions of the developing embryo. Their precise expression patterns act like zip codes to direct where heart muscle, nerve, bone, and other tissues should form, helping to establish the organism’s body plan.
The new research suggests that the Hox genes’ previously unreported role later in life may help keep pools of periosteal stem and progenitor cells at the ready in the bone’s outer periosteum membrane. These available replacement cells can then help maintain healthy tissue and heal broken bones, again in a highly location-dependent manner.
“Our data revealed a previously unknown function for Hox genes as essential location-specific regulators of stem cell maturity in adulthood, with short-term local increases in their expression able to drive healing,” says study senior author and orthopedic trauma surgeon Philipp Leucht, MD, PhD.
In the adult skeleton, he and colleagues found, Hox genes are highly expressed by periosteal stem and progenitor cells but not by more mature cell types like osteoblasts.
The research team showed that a deficiency in Hox genes spurs a decrease in the abundance and proliferation of skeletal stem cells, and an increase in their propensity to differentiate into more mature cell types. In a mix of stem and progenitor cells grown in culture, conversely, increasing the expression of the Hoxa10 gene reduced the cells’ tendency to differentiate and increased their capacity to self-renew.
“The therapeutic promise of adult stem cells as a source of bone-making cells in healing-compromised people is massive.”
When they differentiate, skeletal stem cells give rise to progenitor cells with more limited lineage options and defined lifespans. Here too, the researchers found that overexpressing the Hoxa10 gene yielded dramatic results: The transcription factor drove a reprogramming process that reverted a significant fraction of skeletal progenitor cells to a more primitive, self-renewing stem cell–like state.
Location-Specific Hox Code Governs Bone Repair
As in the embryonic development process, the reprogramming seemed to be highly location dependent. The reversion to more naive stem cells, they found, was restricted to adult stem cells from the same anatomical region where the corresponding Hox genes are expressed, like the Hoxa10 gene’s preferential expression in the tibia and the Hoxa5 gene’s preferential expression in anterior ribs.
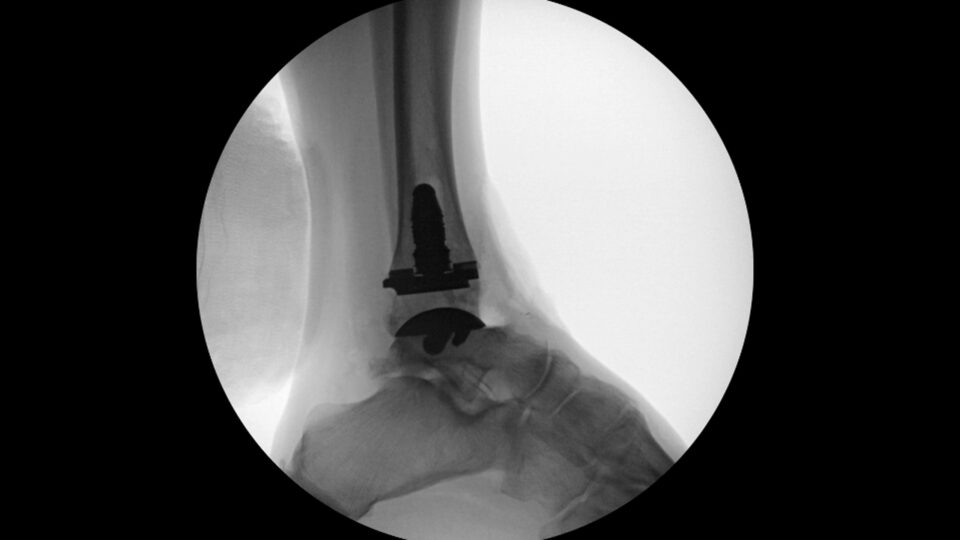
In support of the group’s previous research demonstrating a loss of functional skeletal stem cells with age and an undermining of the skeleton’s regenerative capacity, the new study showed a coincident reduction in Hox expression with age. In mice, they discovered, temporarily overexpressing Hoxa10 partially restored some of the age-related loss in the skeletal tissue’s ability to heal a tibia fracture.
If borne out by more research, clinicians might be able to reprogram the more prevalent progenitor cells in adult skeletal tissue and return them to a more primitive state. The newly converted cells, in turn, could help replenish declining skeletal stem cell populations and improve the bone-healing process in older or repair-compromised patients.
“The therapeutic promise of adult stem cells as a source of bone-making cells in healing-compromised people is massive,” Dr. Leucht says.