Case Highlights:
- A patient with a history of seizures was diagnosed with a 9 mm left temporal AVM, which showed evidence of past bleeds.
- Surgical resection was recommended, but the AVM’s location in an eloquent region related to speech raised the risk of significant sequelae.
- To minimize the necessity of manipulating tissue in the dominant lobe, surgeons performed a pioneering transorbital AVM surgery.
- The procedure was successful, with no complications, and the patient remains seizure-free.
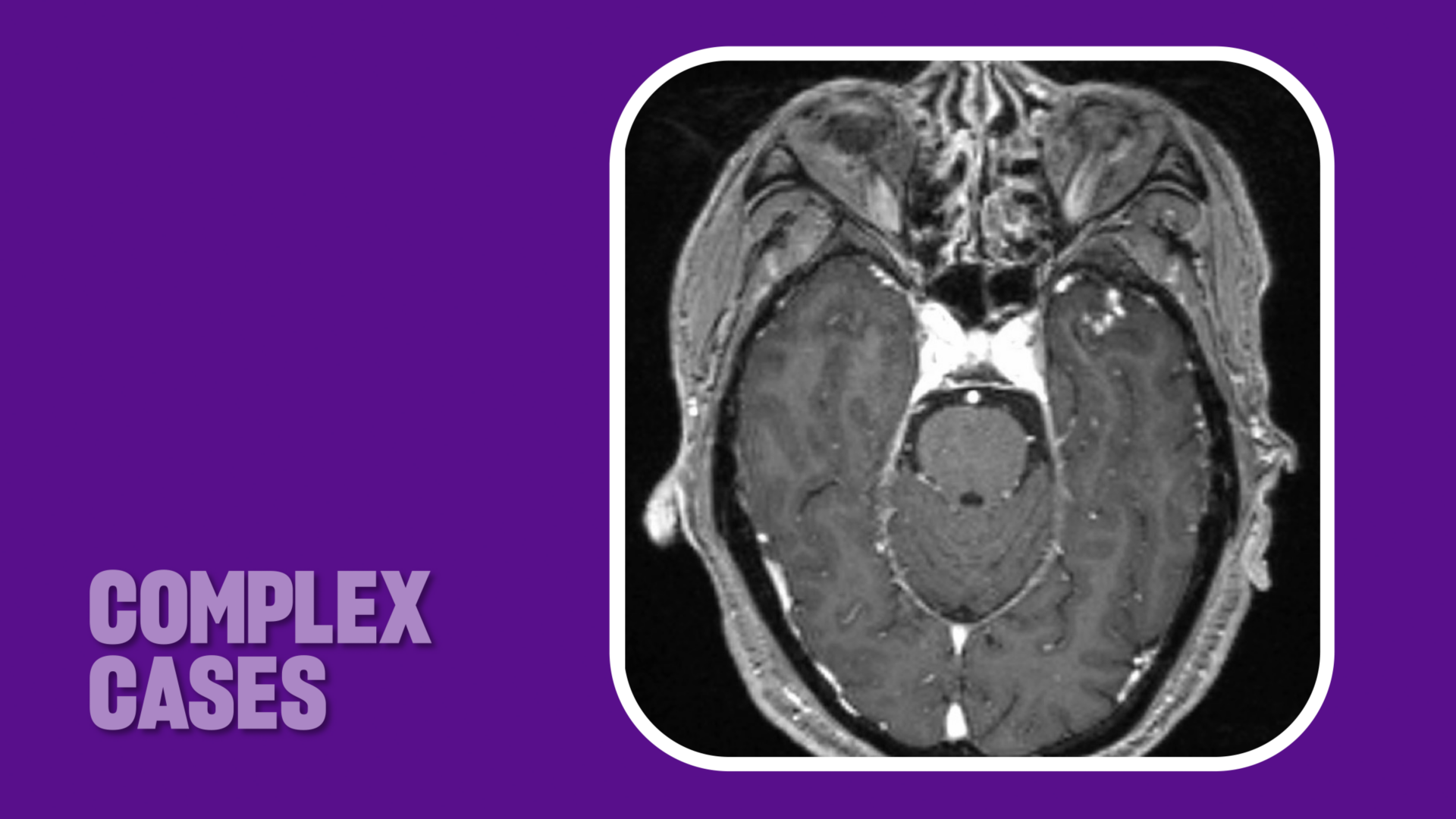
In 2019, a man in his 60s was referred to NYU Langone Health with a history of seizures. Diagnosed with a grade 2 arteriovenous malformation (AVM) in the anterior left temporal lobe, he declined surgical treatment, fearing the risk of damage to speech and language centers in that brain region. Instead, he opted for conservative management, which initially controlled his symptoms.
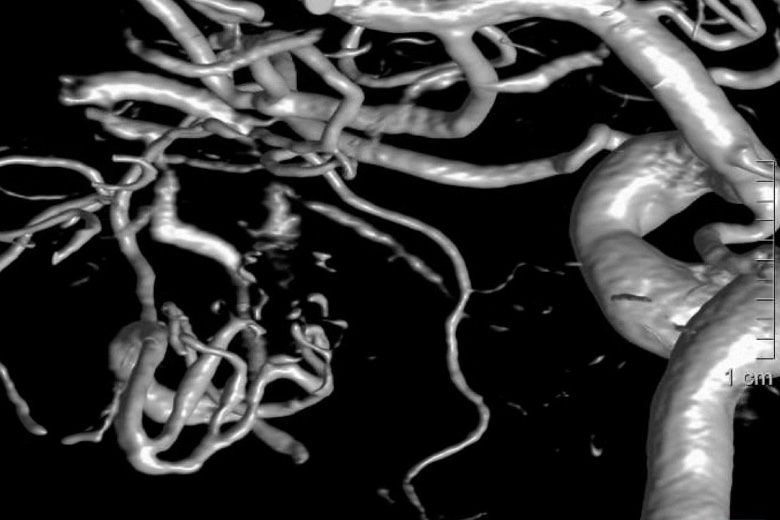
By October 2024, however, his seizures had begun to recur. Diagnostic angiography revealed that the AVM now measured 9 mm in diameter, significantly smaller than its original dimensions. Additional imaging suggested that it had ruptured and bled—and that it might do so again, with potentially catastrophic consequences.
Given this risk, vascular neurosurgeon Erez Nossek, MD, judged surgical resection, rather than radiosurgery or embolization, to be the best therapeutic course. Traditionally, that would mean an open craniotomy. However, Dr. Nossek suggested a novel approach: transorbital surgery.
“I thought a transorbital approach could provide access to the AVM in its most superficial aspect and help minimize the risk of surgical damage.”
Erez Nossek, MD
To date, this minimally invasive technique has mainly been used for skull base tumors. Yet the AVM’s location meant that it might be accessible through the ocular orbit, reducing the need to manipulate eloquent speech tracts in the dominant lobe. “I thought a transorbital approach could provide access to the AVM in its most superficial aspect and help minimize the risk of surgical damage,” he explains.
After the patient expressed interest in exploring this option, Dr. Nossek consulted with a frequent surgical partner, skull base surgeon Donato Pacione, MD, who agreed that it seemed viable—though both specialists knew the challenges would be significant.
Planning an Unprecedented Procedure
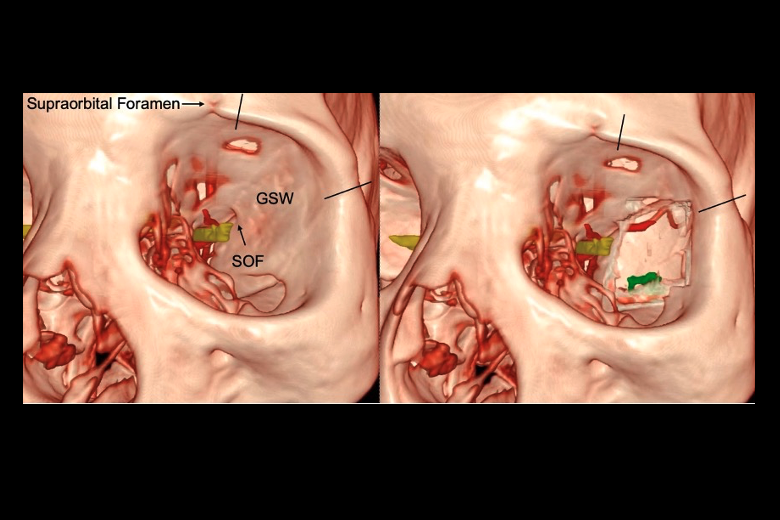
“The main difference between AVM surgery and tumor surgery is the higher risk of bleeding,” notes Dr. Nossek. “If that happens, it’s very difficult to control.” To help plan and execute the complex procedure, Dr. Pacione enlisted neuroradiologist Matthew G. Young, DO, and oculoplastic surgeon Stella Chung, MD. The team plotted the surgical route using 3D virtual reality flythroughs based on CT and MRI scans, then practiced on a cadaver to enhance their preparation.
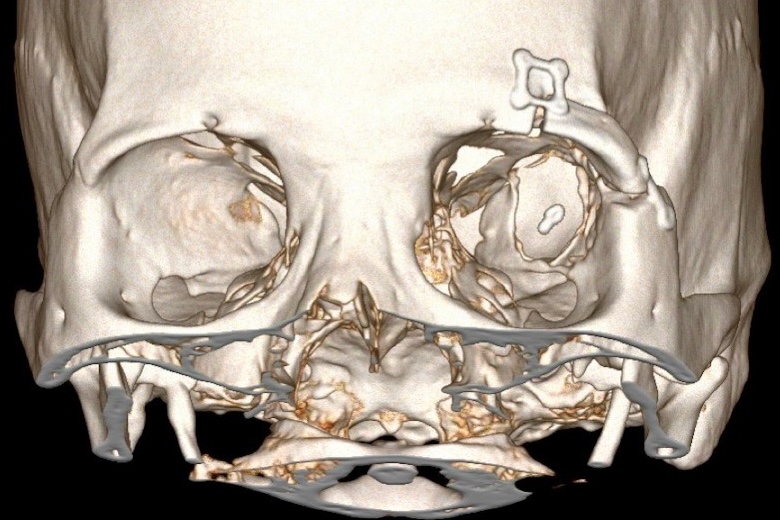
After discussions with the surgeons and his family, the patient consented to the procedure. On February 11, 2025, he was wheeled into a hybrid OR, placed in head pins, and registered to the stereotaxis system. Dr. Chung made the first incision, through the eyelid crease, and the globe of the eye was slightly retracted. Next, Dr. Pacione removed a small piece of the orbital rim. Navigating with an endoscope, he drilled a 2-cm opening at the back of the orbit.
“Our expertise as a team is what made this possible. None of us alone could have made it happen.”
Donato Pacione, MD
Dr. Nossek then took over, guided by a fluorescence-capable microscope. He created a window in the dura, exposing the anterior portion of the AVM. Indocyanine green was used to ascertain the direction of blood flow through and away from the malformation. To avoid rupture, he identified and clipped the main feeder. Then he worked circumferentially around the nidus, using bipolar tools to coagulate and dissect smaller feeders, white matter, and draining veins.
Once the AVM was removed, neurointerventionalist Eytan Raz, MD, PhD, performed an angiogram to confirm that no residual nidus remained. Dr. Nossek reapproximated the dura, and Dr. Pacione inserted a plate and screws to reconstruct the orbit. Finally, Dr. Chung closed the incision in the eyelid.
The patient was discharged two days later, with no complications or visible scarring. Although he remains on anti-seizure medications as a prophylactic, the threat of further brain bleeds has been eliminated.
“Our expertise as a team is what made this possible,” Dr. Pacione says. “None of us alone could have made it happen.”