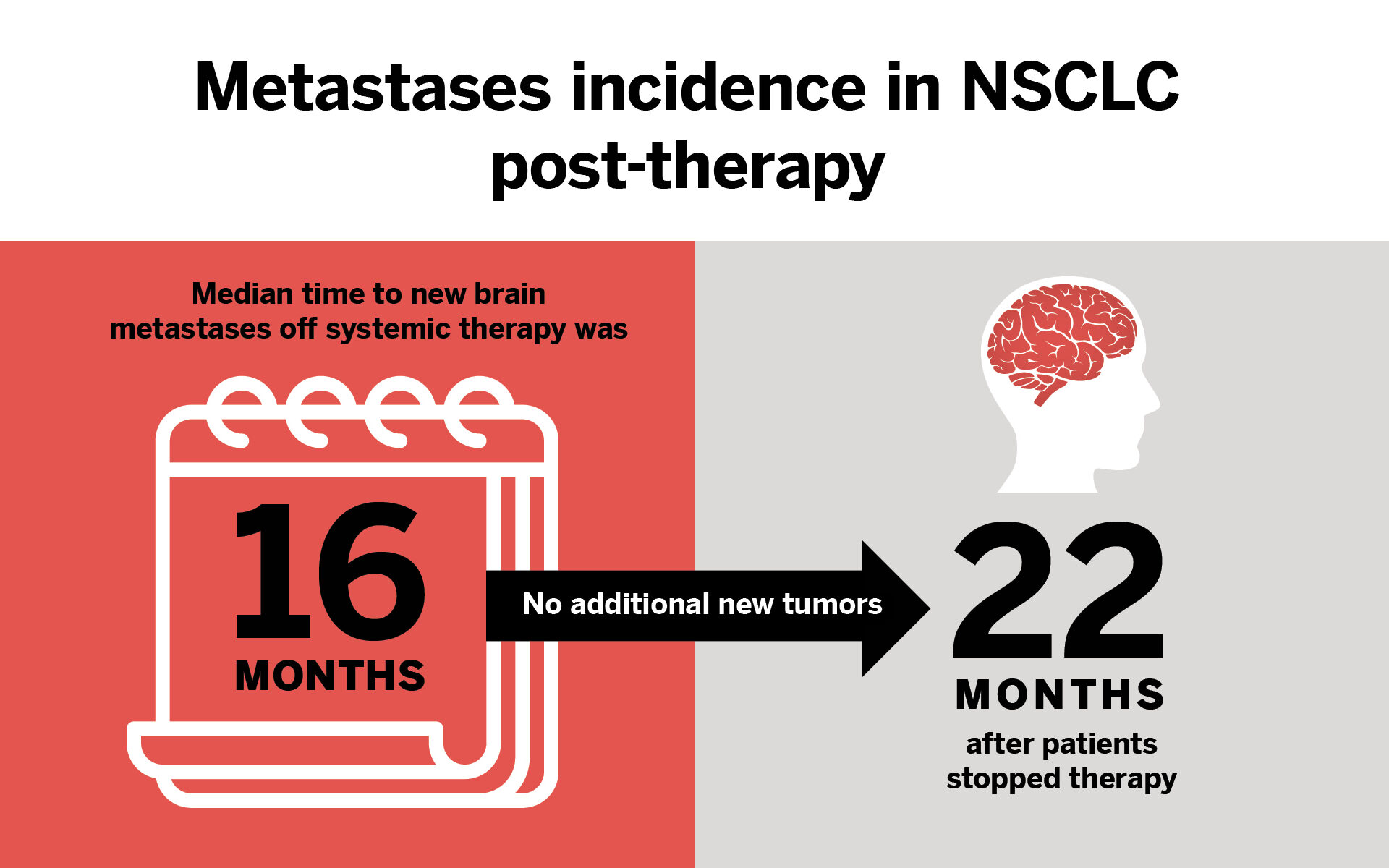
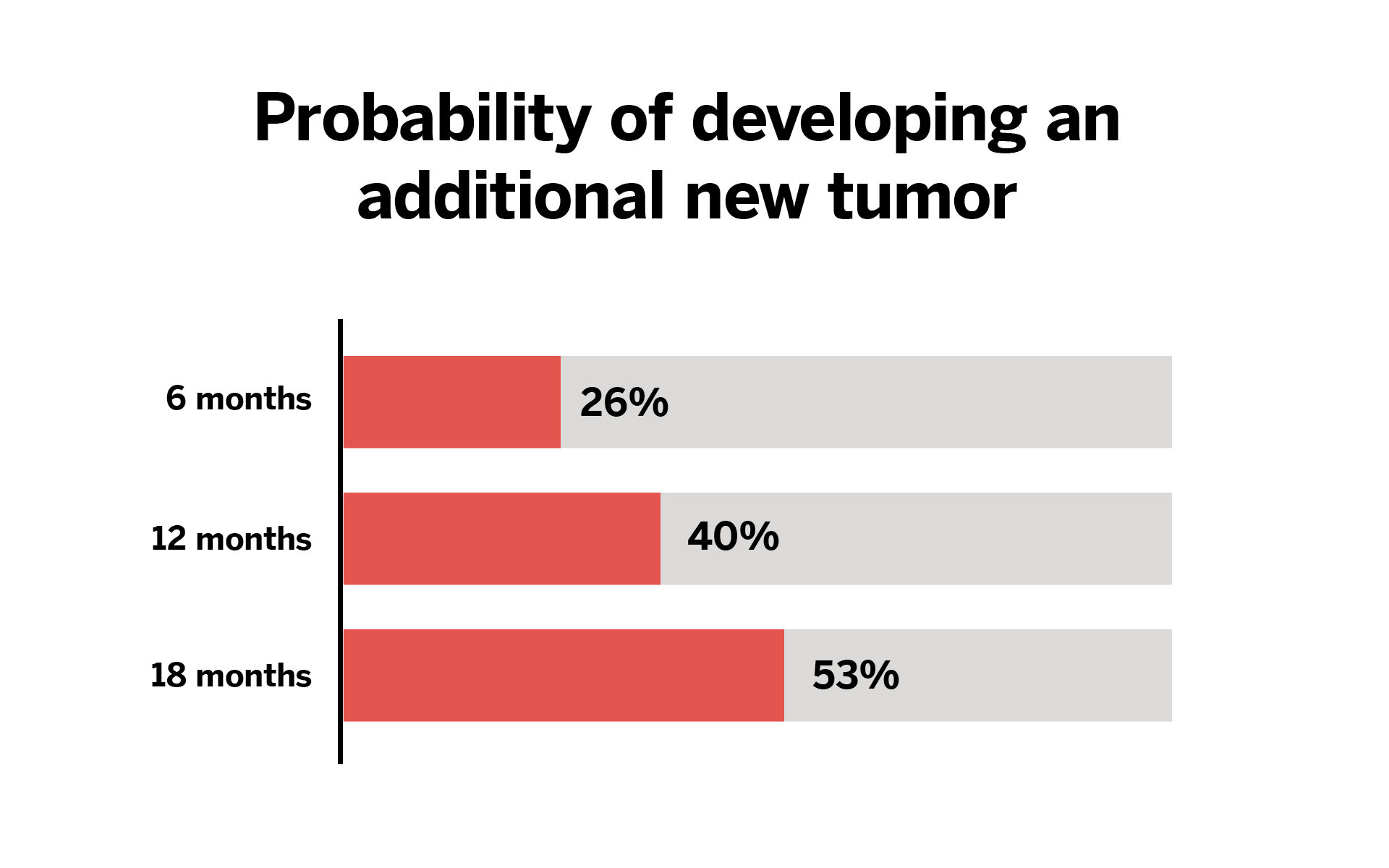
A recent study conducted at NYU Langone Health, published in the Journal of Neurosurgery, has revealed that the rate of new brain metastases from non-small cell lung cancer (NSCLC) in patients off systemic therapy decreases over time and is uncommon two years after discontinuation of systemic cancer therapy.
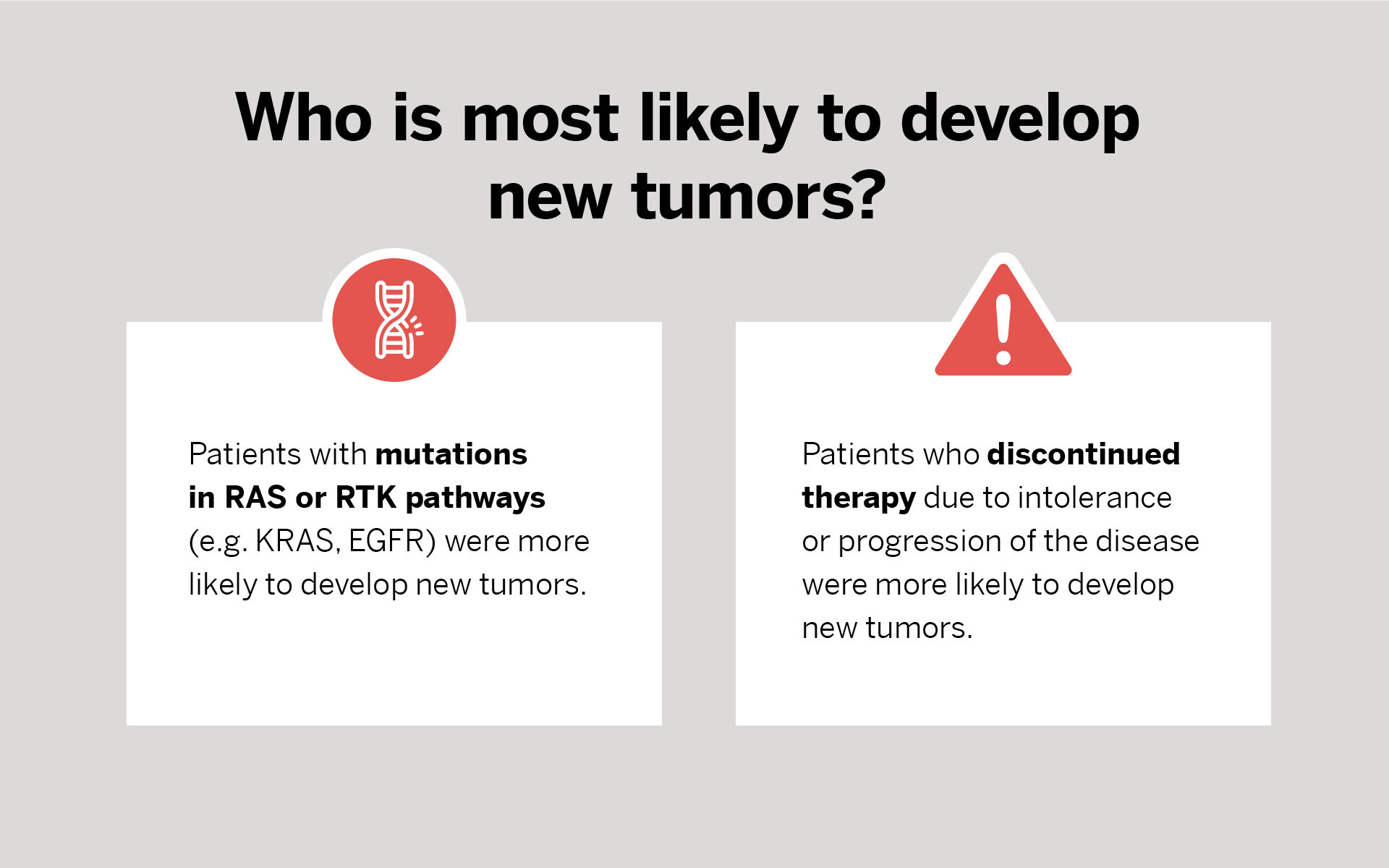
In addition, the researchers found that patients who had RAS or receptor tyrosine kinase (RTK) pathway mutations or who stopped treatment due to adverse events had a higher rate of developing new metastases.
The findings surprised the research team, led by Dennis London, MD, a resident in neurosurgery at NYU Langone.
“Patients who discontinued therapy due to a treatment response had a median time to new brain metastases of 16 months—much longer than we expected,” says Dr. London.
He further explained that these data suggest that the RAS pathway is an aggressive driver of brain metastases in NSCLC, but additional studies with larger sample sizes will be needed to validate this hypothesis.
Based on these findings, Dr. London recommended that oncologists use caution when choosing to discontinue therapy in patients with RAS pathway mutations.
“These data are very encouraging for lung cancer patients with brain metastases,” Dr. London explains. “Achieving long-term neurological control of brain metastases is possible after treatment with new systemic therapies.”
“This is the first study to report the incidence of new brain tumors for patients who can stop their cancer therapy,” says Douglas Kondziolka, MD, a professor of neurosurgery and radiation oncology. “The good news is that for some patients, over years of assessment, new brain tumors were uncommon.”
Fewer Brain Metastases After Stopping Systemic Therapy
Patients who discontinued therapy due to toxicity and those with certain mutations were more likely to develop new tumors.
Featured Experts

Dennis London, MD
Neurosurgery, Epilepsy Surgery
Dennis London, MD, is an assistant professor in the Department of Neurosurgery. His research interests include understanding the function of neural circuitry in action planning and decision-making and applying this knowledge to the treatment of neurologic diseases through neuromodulation; stereotactic and functional neurosurgery; neuro-oncology; and data science.
Dennis London, MD, is an assistant professor in the Department of Neurosurgery. His research interests include understanding the function of neural circuitry in action planning and decision-making and applying this knowledge to the treatment of neurologic diseases through neuromodulation; stereotactic and functional neurosurgery; neuro-oncology; and data science.

Douglas Kondziolka, MD
Neurosurgery
Douglas Kondziolka, MD, is the Gray Family Professor of Neurosurgery, a professor of radiation oncology, and vice chair of clinical research in the Department of Neurosurgery. He is also director of the Center for Advanced Radiosurgery and specializes in metastatic brain tumors, acoustic neuroma, meningioma, primary brain tumors, brain vascular malformations, and other neurologic conditions.
Douglas Kondziolka, MD, is the Gray Family Professor of Neurosurgery, a professor of radiation oncology, and vice chair of clinical research in the Department of Neurosurgery. He is also director of the Center for Advanced Radiosurgery and specializes in metastatic brain tumors, acoustic neuroma, meningioma, primary brain tumors, brain vascular malformations, and other neurologic conditions.
The Best Experts and Latest Breakthroughs
Select your specialty to receive updates on our pioneering research, innovations, expert perspectives, case studies, practice-changing medicine, and more.