Perinatal mood and anxiety disorders are common, with roughly 50 percent of cases in pregnant women going undiagnosed. Of those who receive a diagnosis, only a fraction receive successful treatment. In addition to the considerable effects on maternal and infant morbidity and mortality, there is a large cost burden associated with these disorders, particularly perinatal depression and anxiety.
To begin to close these gaps in diagnosis and treatment, the Department of Obstetrics and Gynecology at NYU Grossman School of Medicine has launched a Perinatal Mental Health Program aiming to strengthen providers’ ability to identify and treat women who are experiencing anxiety, depression, mood disorders, or other mental health issues during the perinatal period.
“Too many women are falling through the cracks, despite the existence of evidence-based treatments.”
Olivia P. Myrick, MD
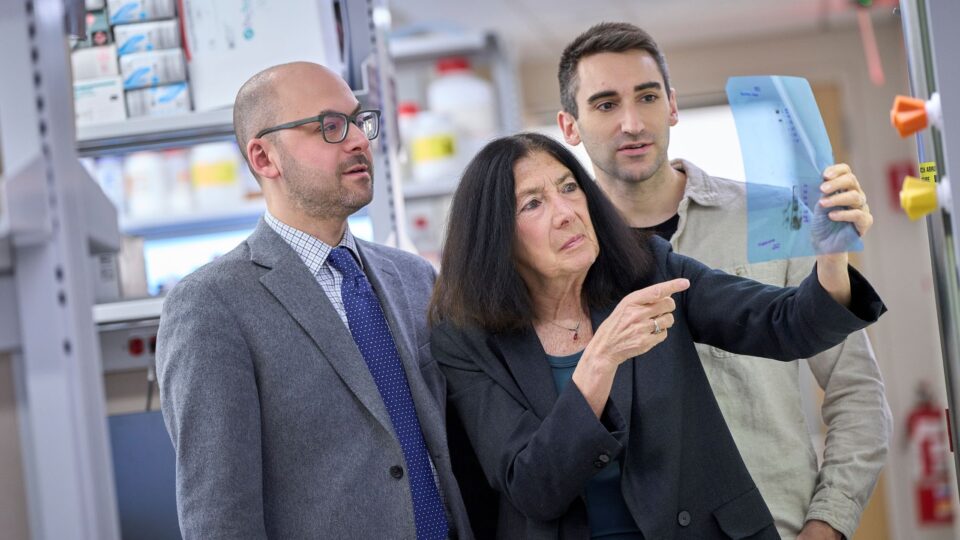
“International guidelines recommend screening for mental health disorders including depression during the postpartum period. However, once the screening is completed, following up with appropriate clinical intervention often does not occur,” says Jessica M. Vernon, MD, director of the new program and a clinical assistant professor of obstetrics and gynecology.
Changing the Postpartum Trajectory
Unfortunately, the limited availability of specialized mental health providers is a significant barrier to integrated healthcare in primary care settings and is especially problematic for pregnant women or those in the postpartum period.
“Common barriers to accessing care include lack of physician availability and issues with insurance reimbursement,” says Olivia P. Myrick, MD, director of education for the Perinatal Mental Health Program and a clinical assistant professor of obstetrics and gynecology. “Very few psychiatrists specialize in pregnant and postpartum women, and few obstetricians are trained to manage psychiatric issues.”
Launched in 2021, NYU Langone’s program has already forged strong collaborative relationships with reproductive psychiatrists and overhauled outpatient workflows, including hiring a new psychiatry fellow to help women with more complex mental health needs and educating obstetric providers on improved screening and treatment initiation. In addition, the program has recruited a dedicated social worker to manage lower-risk patients.
Through the screening process, the providers share referrals and support each other in providing evidence-based, personalized treatment.
Forging Unique Relationships
Additional barriers to mental healthcare in pregnancy include lack of reimbursement and lengthy wait times for psychiatrists. However, these limitation are mitigated through the unique patient–provider relationships within the obstetric care setting.
There is a growing consensus that integrating mental health services into existing service settings, including primary care, is a promising means of increasing access to mental healthcare services; and changes in reimbursement policies can be effective in this regard.
“The model is unique in that it is fully integrated, ensuring that patients will be screened appropriately and reimbursed for provider consultations,” explains Dr. Vernon. “We want everyone to have access to the best-quality care regardless of financial status.”
“The model is unique in that it is fully integrated, ensuring that patients will be screened appropriately and reimbursed for provider consultations. We want everyone to have access to the best-quality care regardless of financial status.”
Jessica M. Vernon, MD
NYU Langone’s perinatal mental health team meets weekly to discuss high-risk patients to ensure they are managed appropriately. With evidence demonstrating the effectiveness of medication and therapy for many perinatal mood disorders, treatment primarily delivered by an obstetric team is optimal, and the direct costs are often reimbursed for patients who are already receiving concurrent prenatal care within the practice.
Expanding the Project Nationally
Today, many obstetrics and gynecology residents and clinicians lack sufficient awareness of mental illness during pregnancy, contributing to the many cases that go unrecognized. Dr. Myrick and Dr. Vernon plan to improve education by launching a series of lectures and by forming partnerships with key stakeholders, such as the National Curriculum in Reproductive Psychiatry, to disseminate these materials broadly.
In the long term, they hope to develop a national curriculum for obstetrics and gynecology trainees, which will be formally published and made available to medical educators.
“Too many women are falling through the cracks, despite the existence of evidence-based treatments,” says Dr. Myrick. “We need to improve access to education, especially for obstetrics and gynecology trainees.”
“The team plans to validate and further refine the model in the coming months, with the potential for telemedicine to be used in the future for diagnosis and treatment.”