Acclaimed pediatric epileptologist Cigdem I. Akman, MD, recently joined Hassenfeld Children’s Hospital at NYU Langone and the Comprehensive Epilepsy Center to launch a dedicated Pediatric Epilepsy Surgery Program. Dr. Akman and pediatric neurosurgeon Eveline Teresa Hidalgo, MD, director of clinical research in pediatric neurosurgery, will co-lead the program to streamline and expand access to NYU Langone’s pediatric epilepsy surgical services.
Here, Dr. Akman shares her plans for the program and her insights on emerging treatment modalities for child and adolescent epilepsy. She also discusses what she has learned over three decades about connecting with patients and their families.
Physician Focus: Dr. Akman, you started out practicing internal medicine in your native Turkey. How did you wind up as a pediatric epilepsy specialist in New York City?
Dr. Akman: Originally, I wanted to study engineering, but my father encouraged me to go to medical school. I’m glad I listened to his advice. After an internship in internal medicine, I decided that my heart was in pediatrics, helping children and their caregivers. So I completed a residency training at Hacettepe University Children’s Hospital in Ankara, Turkey, where I was assigned to pediatric hematology. In 1995, I came to the United States for further training, and found myself strongly drawn to pediatric neurology.
It happened the first time I witnessed a child—an 8-year-old girl—brought to the emergency room for involuntary movements, which were suspected to be seizures. Besides the intensity of her symptoms, what struck me was how terrifying her condition was for her parents and how eager they were to find answers.
A few days later, an evaluation determined that she was having psychogenic non-epileptic events. This news was welcomed by her caregivers, though the therapeutic modalities required to treat her were complex. The incident opened my eyes to how critical it is to make the correct diagnosis—in this case, to distinguish epileptic seizures from symptoms that resemble them—and to provide counseling for patients’ families. That experience on my first day in pediatric neurology consult service made me realize that this was the field for me.
“That experience on my first day in pediatric neurology consult service made me realize that this was the field for me.”
Cigdem I. Akman, MD
Nearly three decades later, I feel privileged to join the superb epilepsy and child neurology team at NYU Langone. In fact, NYU Langone accepted me as a young trainee for an observership in pediatrics while I was still studying in Ankara, so I spent a month here before making the decision to move to the United States. I’m thrilled to be back.
Physician Focus: What’s your vision for the new surgical program at NYU Langone?
Dr. Akman: I’ve always had a special place in my heart for epilepsy surgery, which can be remarkably effective in patients struggling with drug-resistant forms of the disease. Although this treatment modality has been around for more than six decades, it has remained underutilized and is still considered only as a last resort. The persistent misconceptions about this approach—that it is too risky, rarely successful, or only suitable for adults—highlight the work that needs to be done to broaden adoption and improve access to comprehensive care for young patients.
“The persistent misconceptions about [epilepsy surgery]—that it is too risky, rarely successful, or only suitable for adults—highlight the work that needs to be done.”
The Pediatric Epilepsy Program at NYU Langone has long been one of the largest medical and surgical treatment centers of its kind in the country—an accredited Level 4 epilepsy center, recognized for its expertise in providing the highest level of care. By launching a dedicated epilepsy surgery program within this framework, we aim to optimize coordination between the medical and surgical sides of our practice.
The goal is to ensure that children living with drug-resistant epilepsy have access to comprehensive care, and to identify more rapidly those who could benefit from surgical intervention. To that end, I’ll act as a consultant for referring physicians to help facilitate a comprehensive evaluation process to assess patients’ eligibility. If a child is a candidate for surgery, Dr. Hidalgo and I will help our colleagues and the child’s caregivers to develop a treatment plan.
I will also be part of a specialized clinical team in epilepsy to provide services for intracranial EEG monitoring, as well as functional mapping for cortical regions at bedside and in the operating room for patients who are potential candidates for surgery.
Physician Focus: In addition to surgery, what emerging therapeutic approaches are you particularly excited about?
Dr. Akman: Traditional epilepsy surgery aims to remove the epileptic focus to achieve a seizure-free outcome. However, patients with drug-resistant epilepsy for whom surgery is not an option—whether because their epilepsy is nonfocal, or for other reasons—can choose from a growing number of approaches that may reduce the overall seizure burden and decrease the frequency of disabling seizures, thus improving quality of life.
Neuromodulation is increasingly considered as an alternative treatment option for those individuals. Among the various forms of neuromodulation, vagus nerve stimulation is the best known and most established. But responsive neurostimulation and deep brain stimulation are emerging modalities to be considered for pediatric age groups.
We’re also seeing progress in developing treatments for rare epilepsy syndromes that result from mutations affecting a single gene. Early-stage clinical trials are underway for gene therapies aimed at curing these disorders. It’s going to take time, but we’re inching closer and closer.
Physician Focus: Over your three decades as a pediatric epilepsy specialist, what insights have you gained about delivering excellent care?
Dr. Akman: The rewarding thing about pediatric epilepsy is the impact you can make in decreasing seizure burden, preventing related complications, and allowing the child to grow and be independent. By choosing the right therapy, you can profoundly change the course of a young person’s life.
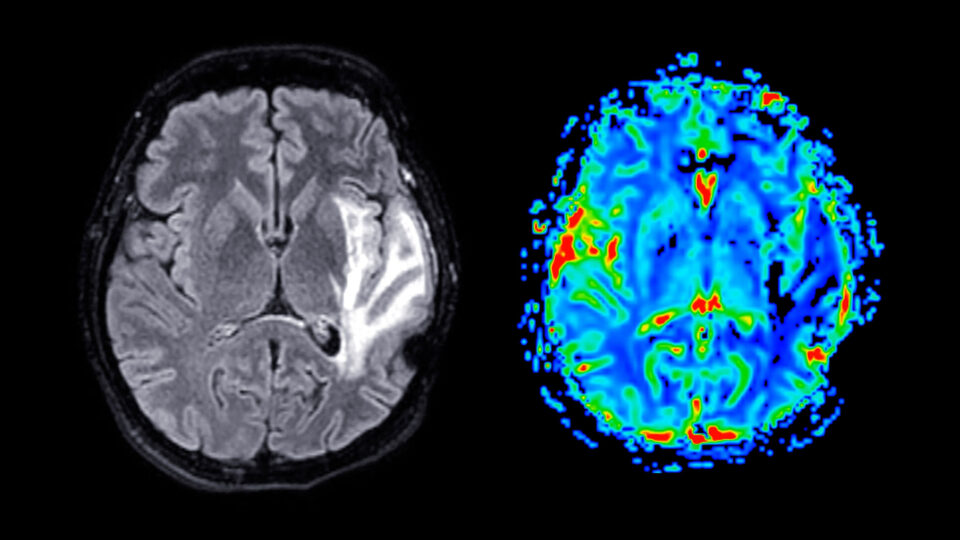
I remember a 5-year-old presenting with seizures characterized by intermittent, severe shoulder pain. Initially, an epilepsy diagnosis was not considered because of the fact that seizures are not painful in general. This child had been admitted to the hospital numerous times for the same symptoms, and she was first evaluated for herpes zoster infection. EEG was later performed to rule out seizure, but it revealed no obvious correlation with her painful events. Her brain MRI was also unrevealing for any structural abnormality. Eventually, however, she received a diagnosis of drug-resistant focal epilepsy based on the persistent, stereotyped clinical events and emerging abnormalities on her repeat EEGs.
“Achieving goals for treating a child with epilepsy depends on teamwork, and on trust built between the patient, caregivers, and physicians.”
The girl underwent intracranial EEG monitoring to determine whether she was a candidate for epilepsy surgery. Her evaluation demonstrated that her seizure focus was located 2 centimeters below the brain surface and localized to the sensory cortex, which resulted in her pain symptoms at the time of seizures. After removal of the epileptic cortex, she became seizure-free. She graduated from college a few years ago and is now studying to become a special education teacher.
This is one of many experiences over the years that helped shape my approach as a clinician. Achieving goals for treating a child with epilepsy depends on teamwork, and on trust built between the patient, caregivers, and physicians. Epilepsy treatment is not one-size-fits-all; it has to be tailored based on the child’s needs and diagnosis. As physicians, we must be careful listeners and observers to establish the right diagnosis, and we must remain open-minded toward treatments with which we may be unfamiliar or lack experience.
It’s also important to understand that caregivers’ perception of treatment options may be affected by cultural, socioeconomic, and religious factors. So communication and transparency are critical elements of epilepsy care. We’ve got to take the time to describe the condition and treatment options thoroughly. When we don’t know the answers, we should be willing to say so. Although being assertive can be difficult, we have to remember that parents can feel overwhelmed by the details and by the responsibility of making tough choices on behalf of their children; it’s our job to help them make a decision.
All this is critical for creating trust. Patients and family members are desperate for someone they can lean on during this difficult journey.