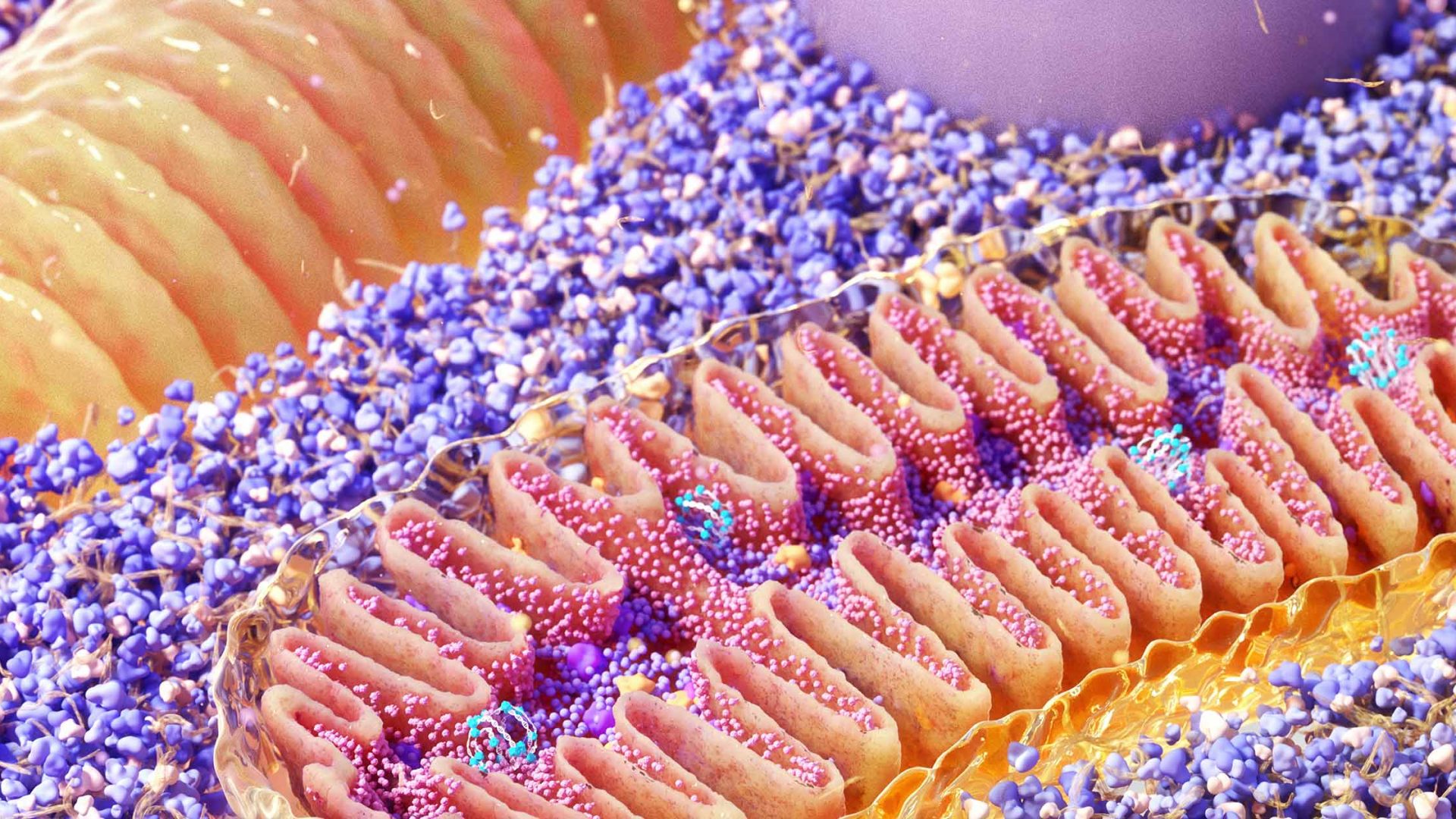
Resistance to venetoclax and other BH3 mimetics in patients with acute myeloid leukemia (AML) occurs due to a rapid increase in mitophagy, the process by which cells break down and turnover mitochondria, according to a new study from investigators at NYU Langone Health and Perlmutter Cancer Center.
Published in Cancer Discovery, the findings build on earlier insights from the team suggesting that targeting mitochondria may serve as a novel approach to overcome venetoclax resistance.
“Our preclinical findings suggest that combining BH3 mimetics like venetoclax with either MFN2 or general mitophagy inhibitors could possibly serve as a future therapy for acute myeloid leukemia.”
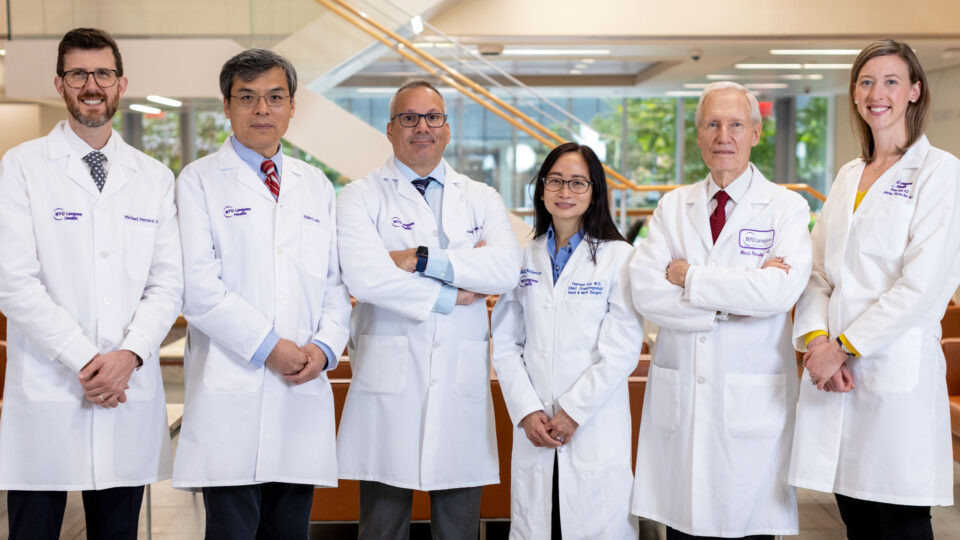
Iannis Aifantis, PhD
“Our preclinical findings suggest that combining BH3 mimetics like venetoclax with either mitofusin 2 (MFN2) or general mitophagy inhibitors could possibly serve as a future therapy for acute myeloid leukemia, as current drug treatments are stalled due to drug resistance,” says study senior investigator Iannis Aifantis, PhD, the Hermann M. Biggs Professor of Pathology and chair of the Department of Pathology.
Specific inhibition of MFN2 is of particular interest as upregulation of the mitophagy regulator was identified as a leading mechanism of venetoclax resistance.
Challenging Resistance
BH3 mimetics function by inhibiting the pro-survival signaling proteins relied upon by cancer cells for unchecked cell growth. Yet, despite their promise for treating AML and other cancer types, resistance arises after prolonged exposure.
Combinatorial BH3 mimetic treatments are being investigated as one approach to improve efficacy; however, experts anticipate resistance to these strategies as well.
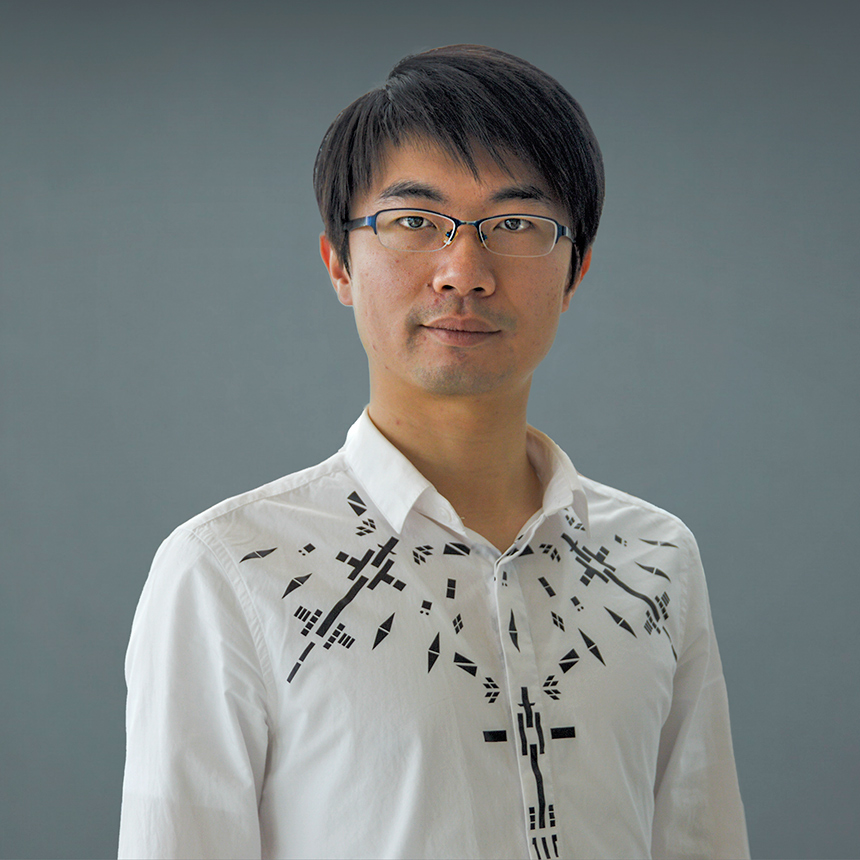
“Acute myeloid leukemia is notoriously difficult to treat, with fewer than a third of those affected living longer than five years after their diagnosis, so it is important to maximize the impact of existing therapies,” says study co-lead investigator Xufeng Chen, PhD, an instructor in the Department of Pathology.
Christina Glytsou, PhD, a former postdoctoral researcher at NYU Langone and now an assistant professor at Rutgers University, also served as co-lead investigator.
Mitophagy: A New Target
In the new publication, the team describes how mitochondrial clearance represents a key tactic deployed by AML cells to evade cell death triggered by BH3 mimetics.
“Because mitochondria serve as a hub for the transmission of cell death signals, their sequestration through mitophagy effectively silences these alarms,” says Dr. Chen.
“Because mitochondria serve as a hub for the transmission of cell death signals, their sequestration through mitophagy effectively silences these alarms.”
Xufeng Chen, PhD
Compared to healthy volunteers, the researchers report that patients with AML display increased expression of MFN2 as well as several other genes associated with mitophagy. These mitophagy genes are also upregulated in patients with poor responses to BH3 mimetics compared to high responders.
Further analyses showed that genetic ablation or pharmacologic inhibition of MFN2 can sensitize human AML cells to various BH3 mimetics. While in animal models of AML, concomitant administration of a BH3 mimetic together with chloroquine, a general autophagy and mitophagy inhibitor, resulted in delayed AML progression and enhanced survival compared to both single agent–treated and untreated mice.
Trials Ahead
The research team now plans to design a clinical trial to test whether chloroquine, when used in combination with venetoclax, prevents drug resistance in patients with AML.
Future studies will also focus on optimizing MFN2-inhibiting compounds like MFI8, a recently developed small molecule that inhibits mitofusins. The molecule was shown in the new study to enhance the efficacy of BH3 mimetics in in vitro AML experiments.
Disclosures
Dr. Aifantis has received research funding from AstraZeneca.