Charles R. Marmar, MD, the Peter H. Schub Professor of Psychiatry, where he is chair, sat down with Marc K. Siegel, MD, at Doctor Radio on Sirius XM to discuss the current mental health crisis and the future of psychiatry treatment. Sirius XM subscribers can hear the full conversation; the extract below has been edited for length and clarity.
Dr. Siegel: We’re having a mental health crisis in this country. Why? And what can we do about it?
Dr. Marmar: It’s very complicated. I don’t think it’s entirely a crisis. I think it’s partially an awakening. I don’t view it through the lens of a sickness in society. It is true that there are some unique stressors. It is true, for example, that the challenges faced by Gen Z, by young people in middle school, high school, and early college now, are because of the inordinate amount of time they spend on devices.
I was discussing this with my family. They went to see MJ: The Musical this weekend for Mother’s Day. And my 14-year-old granddaughters were saying that they’ve deeply identified with the anxiety and stress that Michael Jackson felt as a public figure, because they are exposed in social media as public figures. They’re not Michael Jackson, they’re not creative geniuses, but they empathize deeply with the fate of people who have no privacy and whose image can be damaged or destroyed through the flick of a button. So that does account for new forms of social anxiety, but with it comes a much deeper social awareness.
“The notion of mental health and emotional stress and anxiety and depression has become normalized and part of society and part of primary care.”
Charles R. Marmar, MD
When you and I were children, if we didn’t feel well, we went to see the school nurse. What [children now] do when they don’t feel well is they go to speak to the school psychologist. The notion of mental health and emotional stress and anxiety and depression has become normalized, and part of society and part of primary care.
Dr. Siegel: You’re a leading expert on post-traumatic stress disorder. What’s going on in the world right now in terms of post-traumatic stress, and what can we learn from it?
Dr. Marmar: Well, the world has always been troubled. It’s not clear to me that rates of trauma exposure are necessarily higher now than they were. I mean, after all, if you go back through historical periods when we lived more in tribal structures, we were very prone to illness and predatory forces of animals. We had very little protection against powerful acts of nature.
We’ve always lived in a dangerous, uncontrollable, and unpredictable world. Most of us have seen the Oppenheimer movie. The threat of nuclear war is the threat of existential threat to all of humanity. There are new threats, for sure, but 2 percent of the entire world’s population was killed during World War II. So, we’ve always lived in very dangerous times.
Dr. Siegel: You’re working on precision medicine, which is applying personalized solutions using genetic understandings of variations and differences. How does that apply to post-traumatic stress disorder? Can artificial intelligence help you?
Dr. Marmar: We use it in precision medicine, or at least we use a somewhat more limited version of it, machine learning. So in our precision medicine studies of post-traumatic stress, we ascertain blood-brain imaging studies, cognitive studies, and others. We may have 2 million features to look at in each individual. And we use machine learning programs like Random Forest [classifiers] to find which of those features carries a signal to help us use drug A versus drug B. So that’s a simpler-use AI.
“At the really creative edge, AI is being developed to create psychotherapy avatars.”
At the really creative edge, AI is being developed to create psychotherapy avatars. I’ve seen an example of one being developed by [the U.S. government’s Defense Advanced Research Projects Agency, in which you sit down with this AI avatar and you tell them how you’re feeling. I did that, and they responded to me. My initial experience of the avatar’s response was that it was about as good as an empathic therapist.
Dr. Siegel: That’s pretty good.
Dr. Marmar: That’s not bad. And by the way, think about how stigma-reducing that is. If you’re an active-duty military personnel, who would you rather talk to, Charlie Marmar or talk to an avatar?
Dr. Siegel: What about the way that you’re going to apply precision medicine in a family therapy unit or in a clinic? How is it going to be applied in psychiatry?
Dr. Marmar: One thing we need to be able to do is we need to be pragmatic. Millions of molecular features on each person in routine clinical care will have to be targeted. Ideally, what we would like to do is find those features in blood that are reliable enough to inform diagnosis and guide treatment for stress, anxiety, depression, alcohol, drug abuse, personality challenges, and so on, and have them be simple, affordable, and accessible enough that you, as an excellent primary care doctor, can bake them into your annual blood panel.
So, you’ll get lipids, you’ll get liver-function tests, renal-function tests, and you’ll get psychiatry precision medicine tests. And they will just be part of a routine exam. And when you send your patient to the lab, we’ll get those marked.
Dr. Siegel: What tests am I going to do in the blood? I’m going to check serotonin levels, dopamine levels?
Dr. Marmar: We’re working on it. If I didn’t hold a patent on it, I would talk to you about it.
Dr. Siegel: What does the future hold for alcohol use disorder?
Dr. Marmar: First to say about alcohol use disorder, it’s very profound. It’s very prevalent. It takes a huge number of lives every year. It is horribly disorganizing to a person’s life, health, and career. And there are terrible tragedies from alcohol use disorder.
We have new treatments, of course. We have [Alcoholics Anonymous], AA, and we have some therapies that are very helpful, but we have FDA-approved medications. We have three of them right now: acamprosate, disulfiram, and naltrexone. We have new ones in development. And there is great hope that we will be able to have precision medicine. I’m doing a large precision-medicine clinical trial to determine for whom topiramate, an anticonvulsant, is the best treatment for stress and alcohol.
Dr. Siegel: Where are we heading in mental health?
Dr. Marmar: We’re heading to, first, a major societal change in which mental health challenges such as stress, anxiety, and depression are considered part of life in the way infection and physical injury are considered part of life. They’re baked into mainstream medicine, and they will no longer carry stigma and shame. And children who are being anxious will go to their school counselor and not go to their school nurse with headaches and backaches and other difficulties, which are a proxy for their emotional problems. So it’s going to be normalized. It’s going to be part of primary care.
One out of three of your patients in your primary care practice every day has a primary or secondary mental health problem, and it’ll be part of everyday medicine, and people will feel comfortable to disclose it.
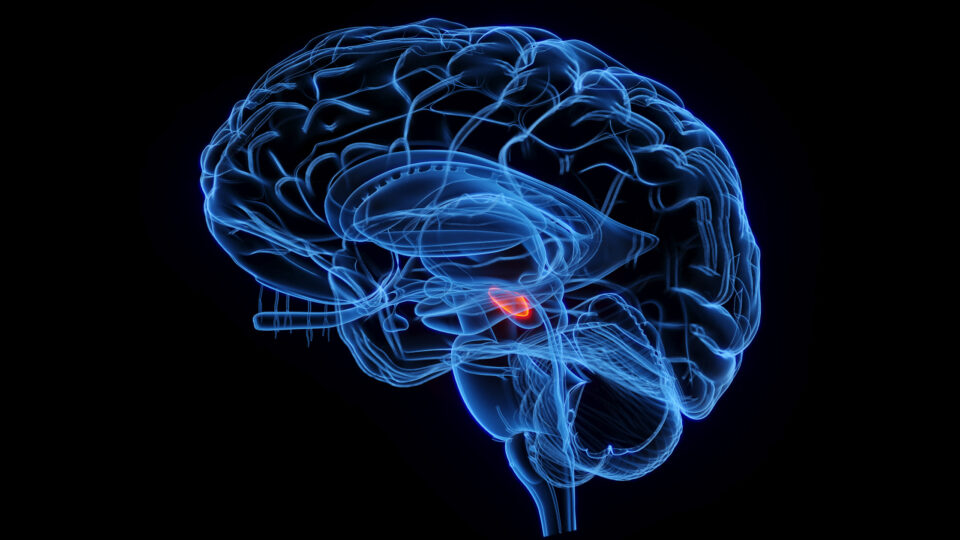
Second, we’re going to have safe and specific treatments, not just psychotherapy, not just medications, but direct ways to modulate the circuits in the brain to relieve these conditions.