Despite the improved survival rate for patients with breast cancer over the past several decades, disparities in mortality rates between White and Black patients have not changed, and a significant gap still exists.
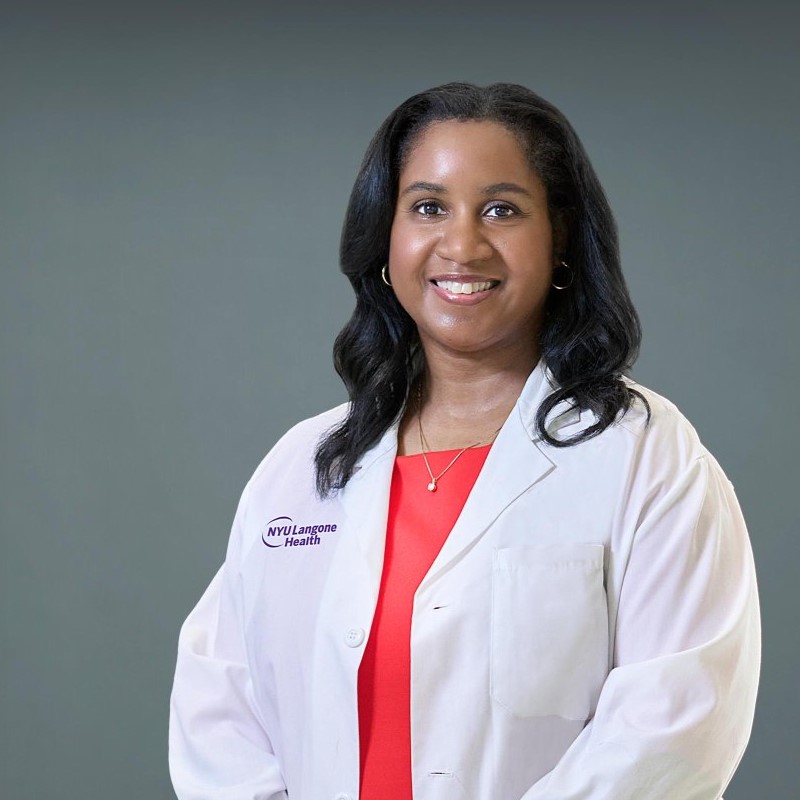
Breast surgeon Kathie-Ann Joseph, MD, MPH, is focused on eliminating this gap.
Here, Dr. Joseph, who serves as clinical systems lead for NYU Langone Health’s Institute for Excellence in Health Equity and co-director of the Beatrice W. Welters Breast Health Outreach and Navigation Program at Perlmutter Cancer Center, reflects on how the recent updates to screening recommendations impact Black women and spotlights an often-overlooked tool: the early risk assessment.
Changing Guidelines Prompt Questions
Physician Focus: The screening guidelines for mammograms have changed over the last few years. Can you share why you think these changes don’t go far enough?
Dr. Joseph: Last year, the U.S. Preventive Services Task Force (USPSTF) lowered the age at which all women can begin breast cancer screening to 40.
It’s great that the USPSTF lowered the screening age for all women, but the recommendation is still for screening every other year. Plus, the guidelines make no mention of risk assessment. If you have a family history, you’re not going to wait until 40, you may need to start screening earlier, you may need to get genetic testing, you may need additional breast imaging, such as an MRI.
“All women, and particularly Black women, need to have a discussion with their primary care doctors no later than the age of 30 about what their risk is for developing breast cancer.”
Kathie-Ann Joseph, MD, MPH
All women, and particularly Black women, need to have a discussion with their primary care doctors no later than the age of 30 about what their risk is for developing breast cancer so that they know when they should start screening.
Primary Care Conversations
Physician Focus: Your research focuses on disparities in screening and diagnostic follow-up care in Black women. What does this research tell us?
Dr. Joseph: Our research has found that Black women tend to be diagnosed with breast cancer at a younger age than White women and have a 42 percent greater risk of death from breast cancer than White women if diagnosed before age 50. They are also more likely than White women to get a diagnosis without having had a single screening exam.
Before the guidelines changed, I and a group of breast surgical oncologists led a multicenter study published in the Annals of Surgical Oncology that advocated that Black women needed to be screened earlier. Because Black women experience higher rates of breast cancer diagnoses before age 50, and are at greater risk for more-aggressive disease, initiating risk assessments and screening earlier can make a significant impact on closing those care gaps.
“Primary care physicians must inquire about a patient’s family history of cancer, even though it’s not something typically discussed among family members in the Black community.”
We also found there’s education that needs to happen with primary care doctors and obstetrician–gynecologists.
Sometimes we see young women with breast cancer who have multiple family members with breast cancer but have never been referred for genetic testing. Primary care physicians must inquire about the family history of cancer, even though it’s not something typically discussed among family members in the Black community. Not initiating conversations with Black women about family history, risk, and screening opportunities perpetuates the current care gaps.
Community Engagement to Improve Screening
Physician Focus: Your team is working to identify and educate underserved women who would benefit from breast cancer screening. Can you talk more about the Beatrice W. Welters Breast Health Outreach and Navigation Program?
Dr. Joseph: The program started as purely community engagement, but it morphed into something much bigger.
We started by placing nonclinical patient navigators in the community, engaging women where they work, live, and socialize. The goal is to help educate women in the community on their risk and care options and then help them schedule appointments for mammograms and further diagnostic screening if needed. If they are diagnosed, that same navigator helps them along their entire cancer journey, including access to services if they are uninsured.
As word spread among other community-based organizations, it became clear that some women who are diagnosed with breast cancer don’t have the means to travel in for treatment or deal with insurance issues. Now, we not only have navigators out in the community educating women at churches and beauty salons, but we also have navigators in our clinics in Brooklyn and Bellevue assisting patients with travel plans, insurance claims, and more. So far, we’ve had over 20,000 encounters.
“We not only have navigators out in the community educating women at churches and beauty salons, but we also have navigators in our clinics.”
Genetic testing and counseling are also part of the Welters Program; we felt it was important to have this available for all our patients, especially those who lack health insurance. We have two dedicated genetic counselors and a genetic counseling assistant as part of our program.
Physician Focus: If there’s one takeaway message from your work in this area, what would that be?
Dr. Joseph: Physicians should be vigilant about conducting breast cancer risk assessments for all women, but Black women are at an increased risk. It is important for them to not only get screened and examined annually beginning at 40, but they also need to have a risk assessment done no later than the age of 30.