A recent study by researchers at NYU Langone Health provides some of the first evidence that SARS-CoV-2 can directly infect coronary tissue, including coronary immune cells. Their findings, published in Nature Cardiovascular Research, shed mechanistic insight into how COVID-19 infection contributes to elevated risk of ischemic cardiac events in individuals with atherosclerosis.
“This is the first evidence of a possible direct linkage between SARS-CoV-2 infection, the inflammatory response, and cardiovascular events.”
Chiara Giannarelli, MD, PhD
“This is the first evidence of a possible direct linkage between SARS-CoV-2 infection, the inflammatory response, and cardiovascular events,” says study senior author and cardiologist Chiara Giannarelli, MD, PhD.
COVID-19 and Cardiac Risk
SARS-CoV-2 infection increases the risk of acute myocardial infarction and stroke for up to a year after the initial infection. Cytokine storms—an extreme inflammatory response arising from infection—are presumed to be a factor. But what happens at the cellular level in the vasculature?
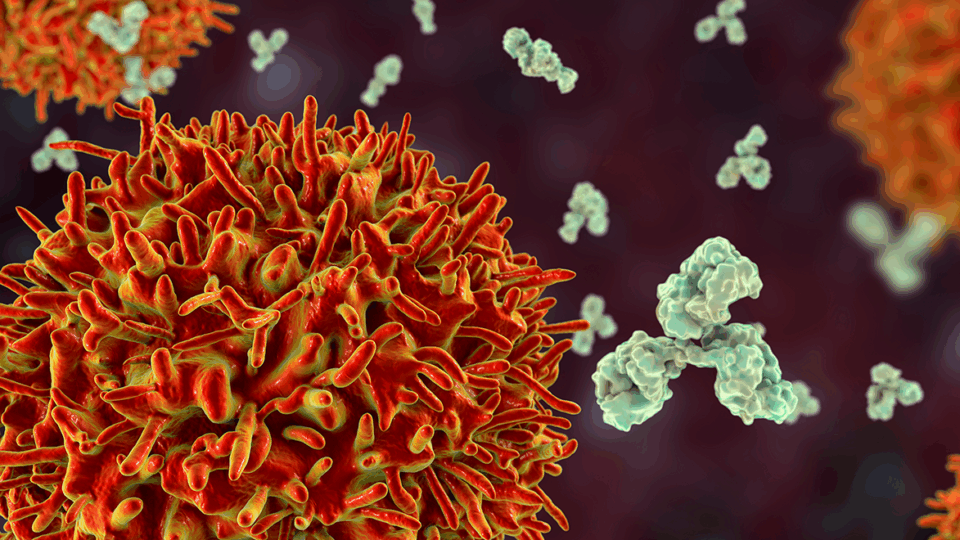
The new study was designed to uncover any direct impacts on the coronary vasculature, and researchers hypothesized that immune cells, such as macrophages, could be involved.
Artificial Intelligence Amps Up Viral Detection
Their analysis detected the virus within the arteries of eight men and women with a history of atherosclerosis who had died of COVID-19. The authors trained a neural network artificial intelligence program to measure viral RNA levels, specifically in cells infiltrating the arterial wall.
In addition to infecting arterial tissue, viral RNA was also detected in infiltrating macrophages. “This study definitively shows that SARS-CoV-2 can infect and replicate in macrophages in the coronary vasculature of individuals with COVID-19,” says Dr. Giannarelli.
“This study definitively shows that SARS-CoV-2 can infect and replicate in macrophages in the coronary vasculature of individuals with COVID-19.”
Viral replication levels were highest in samples classified as “pathological intimal thickening with macrophage infiltration”—believed to be the precursor phase to atherosclerotic plaque formation.
Preferential Infection of Foam Cells
Not all macrophages appear to be equally susceptible to SARS-CoV-2 infection. The study findings revealed that macrophages rich in engulfed fat, called foam cells, were infected more frequently and for longer periods than typical macrophages.
According to the researchers, this suggests that the coronavirus may persist more easily in people with large amounts of plaque buildup in their arteries, partly explaining why those with atherosclerosis are more susceptible to COVID-19.
Provoking an Inflammatory Response
The experiments showed that in response to infection, the macrophages release cytokines known to promote a chronic immune response. The researchers note that two identified cytokines, interleukin-1 beta and interleukin-6, are tied to heart attacks.
This heightened state of inflammation may facilitate the formation and rupture of arterial plaques, impeding blood flow, explains Dr. Giannarelli.
Understanding of Long COVID
“These results shed light on a possible connection between preexisting heart issues and long COVID symptoms,” says Dr. Giannarelli. “It appears that the immune cells most involved in atherosclerosis may serve as a reservoir for the virus, allowing it to persist in the body over time.”
“The immune cells most involved in atherosclerosis may serve as a reservoir for the virus, allowing it to persist in the body over time.”
As a result, the research team next plans to explore more closely this potential link between the coronavirus’s behavior during atherosclerosis and long COVID, whose symptoms may include heart palpitations, chest pain, and fatigue.
Dr. Giannarelli adds that because the current study analyzed tissue infected with viral strains that spread throughout New York City early in the pandemic, the authors are investigating any differences after exposure to newer variants and the protective effects of vaccination.