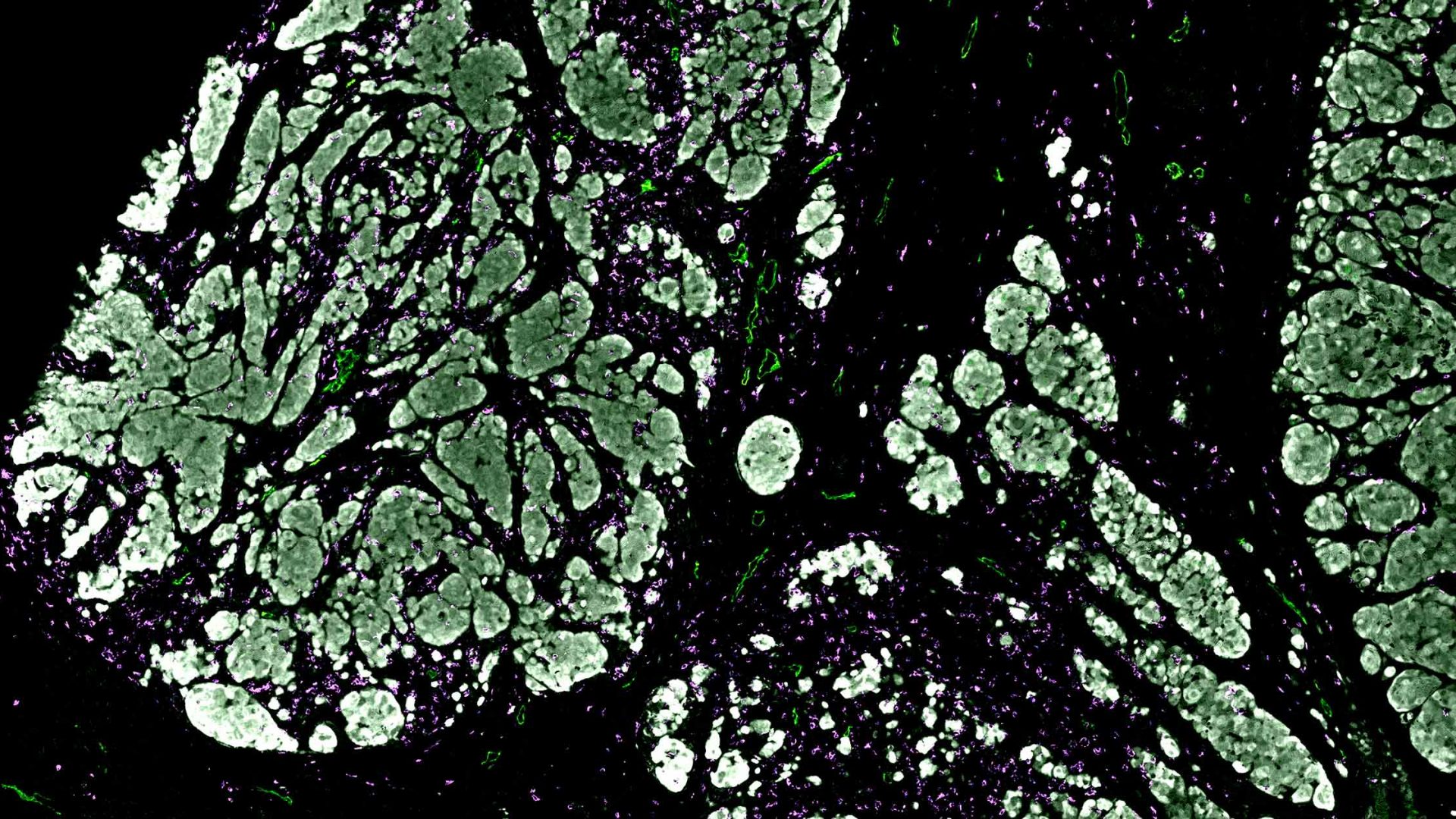
Antigen-specific CD8 T cell accumulation in tumors is crucial for effective immunotherapy. Data indicate that lymphatic vessels and their transport function may impede this process under some conditions. Yet the mechanisms by which lymphatic vessels affect CD8 effector T cell function within the tumor microenvironment (TME) are not well characterized.
In a study published in Nature Immunology, a team led by NYU Langone Health and Perlmutter Cancer Center researchers clarified key aspects of these interactions in melanoma. The scientists also found a way to keep CD8 T cells from exiting cutaneous tumors—and showed that doing so in conjunction with immune checkpoint blockade could significantly decrease tumor growth.
“Our work shows that preventing T cell egress can boost the efficacy of immunotherapy against melanoma.”
Amanda W. Lund, PhD
“Our work shows that preventing T cell egress can boost the efficacy of immunotherapy against melanoma,” says senior investigator Amanda W. Lund, PhD, an associate professor of dermatology and pathology. Maria Steele, PhD, a former postdoctoral fellow in the Ronald O. Perelman Department of Dermatology, served as study lead investigator.
Pinpointing the Role of Lymphatic Transport
Previous research has shown that CD8 T cells (among other types) can migrate out of tumors into lymphatic vessels. In addition, an earlier study by Dr. Lund and colleagues demonstrated that adoptive T cell therapy for melanoma is enhanced in mice engineered to lack dermal lymphatic vessels compared to wild-type controls.
Such findings led Dr. Lund and her research team to hypothesize that functional lymphatic vessels may limit the efficacy of tumor-specific CD8 T cells by facilitating their exit from the TME. In their new study, the researchers sought to understand how this escape route operated and how it might be interrupted.
The team began by tracking transferred antigen-specific CD8 T cells in vivo in the absence of dermal lymphatic vessels. These cells equally infiltrated melanoma tumors in both lymphatic-deficient and wild-type mice. By day 7 after transfer, however, more T cells had accumulated in lymphatic-deficient tumors, even though their proliferation was lower. These data confirmed that lymphatic transport decreases the retention of therapeutic T cells.
Blocking an Escape Signal
To determine how retention could be increased, the team investigated chemokine pathways whose surface expression was regulated in concert with intratumoral activation and progressive dysfunction. They found that the chemokine CXCL12 and its receptor protein CXCR4 attract CD8 T cells toward the tumor periphery, limiting their target engagement and encouraging their escape into lymphatic vessels.
When the researchers blocked this signaling pathway using the CXCR4 antagonist AMD3100, T cells no longer migrated to the periphery. And with continuous administration of the drug, their numbers within the TME doubled.
These changes suggested that blocking the CXCR4 pathway would also prime the TME for response to immunotherapy. To test the therapeutic impact of AMD3100 in the context of immune checkpoint blockade, the team administered the drug both with and without an anti–PD-L1 inhibitor to mice with established melanoma tumors.
Alone, the CXCR4 antagonist did not have statistically significant effects. In combination with the immune checkpoint inhibitor, however, it arrested growth in approximately half of the tumors. Immunotherapy alone had previously failed to stop the cancer’s proliferation.
“These results suggest that it is not only about getting T cells into the melanoma tumor, but also about getting them to the right place with the right signals to drive the most specific and durable immune responses,” says Dr. Lund.
In future research, the team will investigate other molecular pathways in lymphatic vessels to increase the “dwell time” of CD8 T cells within tumors.
Disclosures
Dr. Lund is a paid consultant for AGS Therapeutics, a biopharmaceutical company that was not involved in the study.