Treatment decisions for voice disorders are largely based on either-or thinking: Is the problem due to injury to the outer vibratory layers of the mucosa or dysfunction of the underlying muscle? But Aaron M. Johnson, PhD, co-director of NYU Langone’s Voice Center, suspects complex interactions between the mucosa and muscle may be in play that could inform new targeted therapies.
“What we’re proposing is that there are mechanistic reactions of the muscle itself in response to chronic phonotrauma of the outer vibratory layers that may lead to functional deficits,” Dr. Johnson says. “So even when we think the cause of the voice problem is superficial injury, targeting the muscle may help treat an underlying, unseen, deeper, problem.”
“What we’re proposing is that … even when we think the cause of the voice problem is superficial injury, targeting the muscle may help treat an underlying, unseen, deeper problem.”
Aaron M. Johnson, PhD
To test this hypothesis and others, Dr. Johnson was recently awarded a prestigious five-year grant of $3.2 million from the NIH.
When Phonotrauma Persists
Injuries to the vocal folds may occur the morning after a night of cheering at a concert, baseball game, or other event, when people often wake up with a sore throat and raspy voice. “All of us experience what we call phonotrauma, which is when we use our voice with a lot of intensity or over a long period of time,” Dr. Johnson explains.
In many cases, the symptoms of phonotrauma resolve with rest. “The fact that we don’t have voice disorders all the time is amazing to me,” Dr. Johnson says, “given our vocal folds collide with each other hundreds of thousands of times each day.”
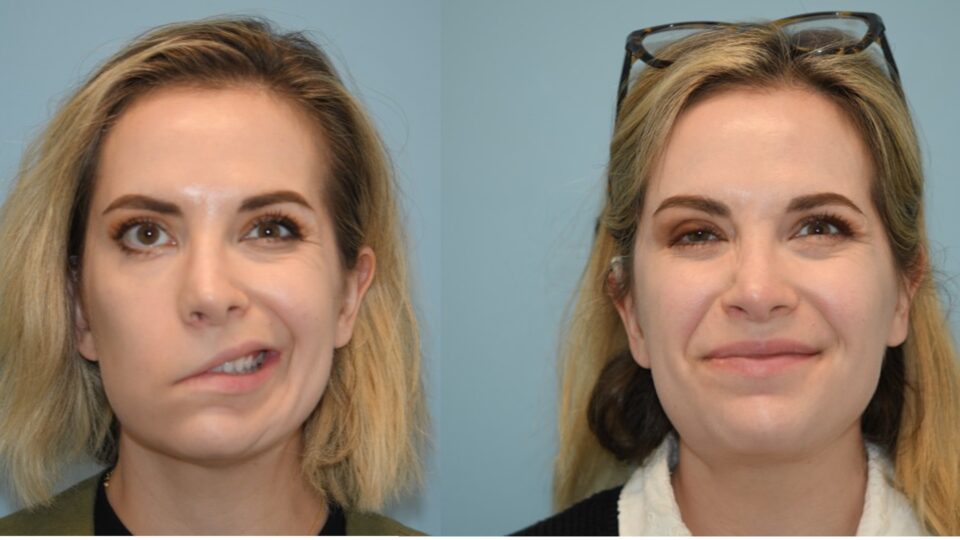
However, repeated phonotrauma can lead to phonotraumatic dysphonia, a specific voice disorder that causes an abnormal or hoarse voice. The disorder often affects those who rely heavily on their voice for their profession, such as teachers, singers, lawyers, and politicians.
If left unaddressed, phonotraumatic dysphonia can further progress into vocal hyperfunction, which involves the dysfunction and tensing of the underlying thyroarytenoid muscle, the primary muscle of the vocal fold, as well as the surrounding musculature in the neck.
Vocal hyperfunction has long been viewed as a natural behavioral response to phonotrauma. “But it can also exacerbate the problem,” Dr. Johnson says, “and create a vicious cycle of people straining more, which causes more phonotrauma, which creates more vocal hyperfunction.”
Mucosa–Muscle Interactions
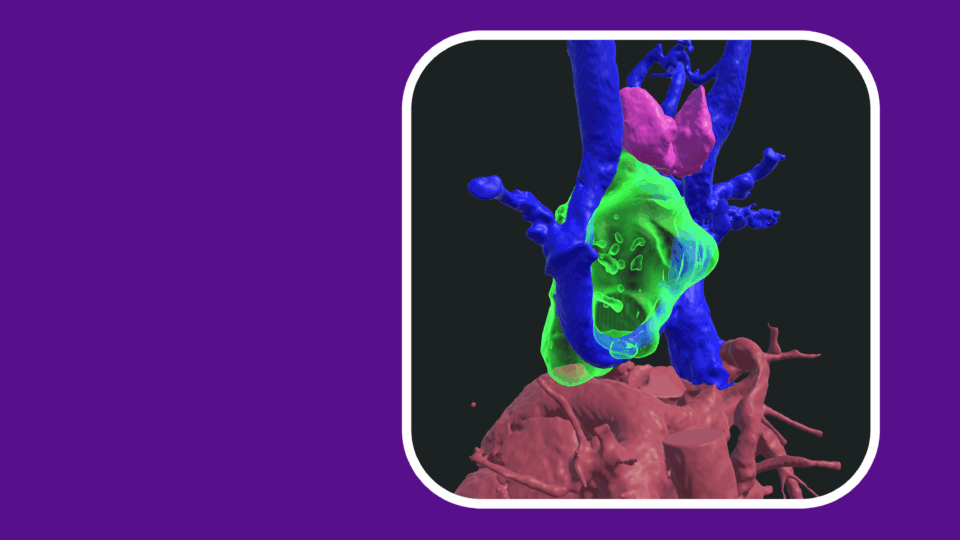
To look more closely at a bidirectional relationship between the mucosal tissue and muscle layers of the vocal fold, Dr. Johnson is collaborating with Ryan Branski, PhD, vice chair of research for otolaryngology—head and neck surgery. The team’s initial in vitro cell–cell interaction studies focused on what might happen when fibroblasts from the mucosa and myoblasts from the muscle commingle.
Published in the Annals of Otology, Rhinology & Laryngology, their findings revealed that fibroblasts have a largely negative impact on myoblasts, potentially leading to a delay in the growth and regeneration of muscle. Conversely, the impact of myoblasts on fibroblasts was positive.
“That study demonstrated that laryngeal myoblasts have a favorable effect on fibroblasts, suggesting that when the laryngeal muscle is healthy it may support a healthy mucosa,” Dr. Johnson says. “On the other hand, when there is muscle dysfunction, that may lead to a deleterious effect on the vocal fold mucosa.”
“That study demonstrated that laryngeal myoblasts have a favorable effect on fibroblasts, suggesting that when the muscle is healthy it may support a healthy mucosa.”
To clarify the mechanisms involved and identify potential therapeutic targets, the team aims to conduct follow-up studies characterizing unique fibroblast–myoblast signals and their interaction with inflammatory cells from the vocal folds.
Elsewhere in the body, researchers have long known that muscle, such as skeletal muscle, is involved in an inflammatory response to injury. But Dr. Johnson says that “really nobody, up until our work, has looked at the response of laryngeal muscle to similar types of injury elicited by phonotrauma.”
A Focus on Vocal Trauma Depth
In another line of experiments, the team aims to compare how the thyroarytenoid muscle responds to both shallow vocal fold injuries and deep injuries that extend into the thyroarytenoid muscle itself. For this work, he and colleagues are leveraging Dr. Johnson’s experience with a unique behavioral model, rodent vocalizations.
Rats communicate via whistles in the ultrasonic range. The vocalizations, which resemble sped-up birdcalls, don’t rely on vibrating vocal folds but rather an air jet that resonates through a hole to create whistling noises. Although not a perfect approximation, the whistling uses the same muscles as human vocalizations, making the system a useful model for looking at neuromuscular changes within the larynx.
In their rat model, the researchers create a superficial injury to the outer vibratory layers of the vocal folds to approximate phonotrauma in humans. A second, deeper injury extends into the underlying thyroarytenoid muscle. The researchers then record the rodents’ vocalizations before and at multiple points after each type of injury to see how depth of injury affects recovery of the vocalizations.
The team suspects that in both conditions, the frequency complexity of the vocalizations will be reduced because of changes in the muscle. They will confirm their vocalization findings with direct ex vivo measurements of the contractile properties of the thyroarytenoid muscle.
Additionally, the researchers plan to compile and compare the full proteome of the thyroarytenoid muscle in both healthy and injured states. In a previous proteomic characterization of laryngeal muscles from rats, Dr. Johnson and collaborators analyzed the relative abundance of roughly 1,000 proteins, demonstrating how the same technique could be applied to do a deeper dive into the extent and nature of muscle changes after vocal trauma.
“Collectively, these studies will help us understand the complex interplay between vocal fold mucosal injuries and the underlying thyroarytenoid muscle and hopefully lead to improved diagnosis and treatment of voice disorders,” says Dr. Johnson.