New research in the Journal of Neurosurgery shows how tumor volume and growth rate affect hearing in patients with vestibular schwannomas, bringing clarity to a contentious topic.
While more than 90 percent of patients with these noncancerous growths present with some hearing loss, many choose not to intervene due to concerns over further impairment. However, even if an acoustic tumor does not grow larger, risks to Class A and serviceable hearing remain.
“Hearing loss can occur with small or large tumors,” says John G. Golfinos, MD, co-director of the Brain & Spine Tumor Center at Perlmutter Cancer Center. “By understanding the relationship between tumor growth and hearing loss, we are better able to choose appropriate management strategies.”
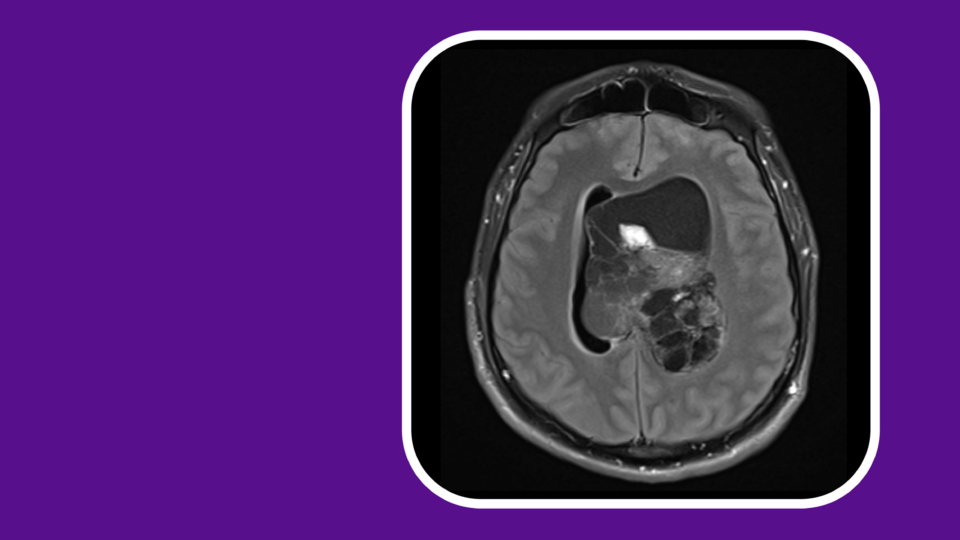
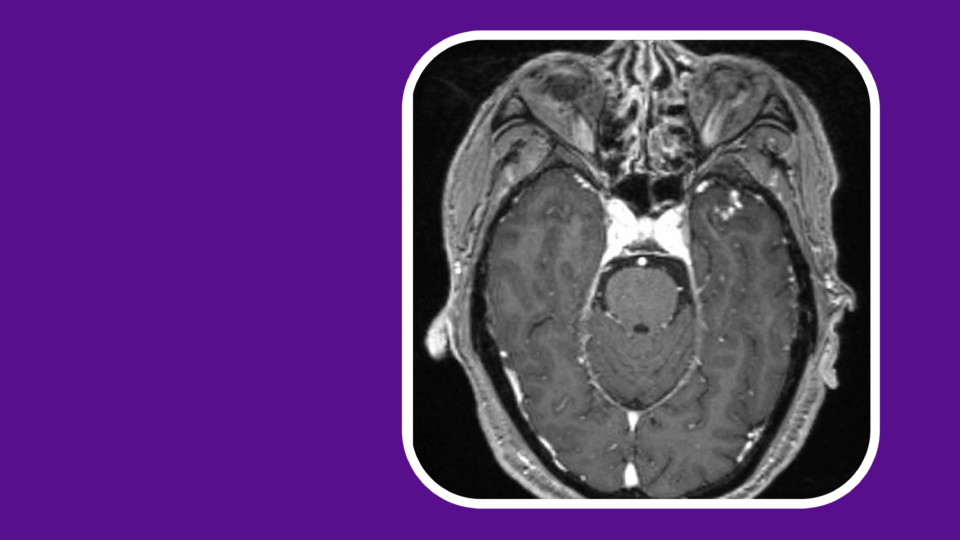
A team at NYU Langone Health including Dr. Golfinos, J. Thomas Roland Jr., MD, and Douglas Kondziolka, MD, analyzed serial imaging and audiometric data from 128 patients with untreated, unilateral vestibular schwannomas. MRI allowed the researchers to calculate total tumor volumes, as opposed to relying on more traditional single-axis diameter measurements.
“By understanding the relationship between tumor growth and hearing loss, we are better able to choose appropriate management strategies.”
JOHN G. GOLFINOS, MD
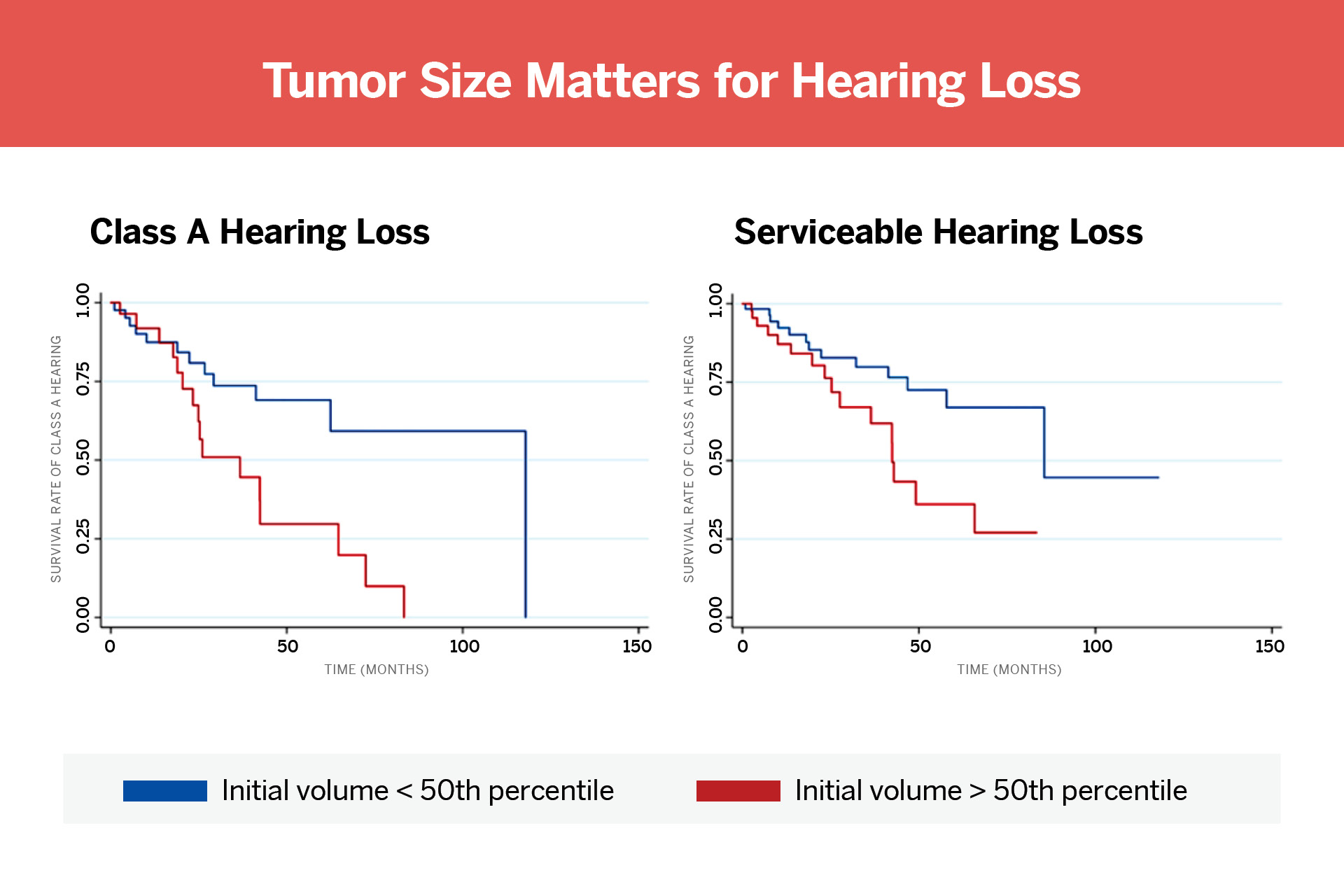
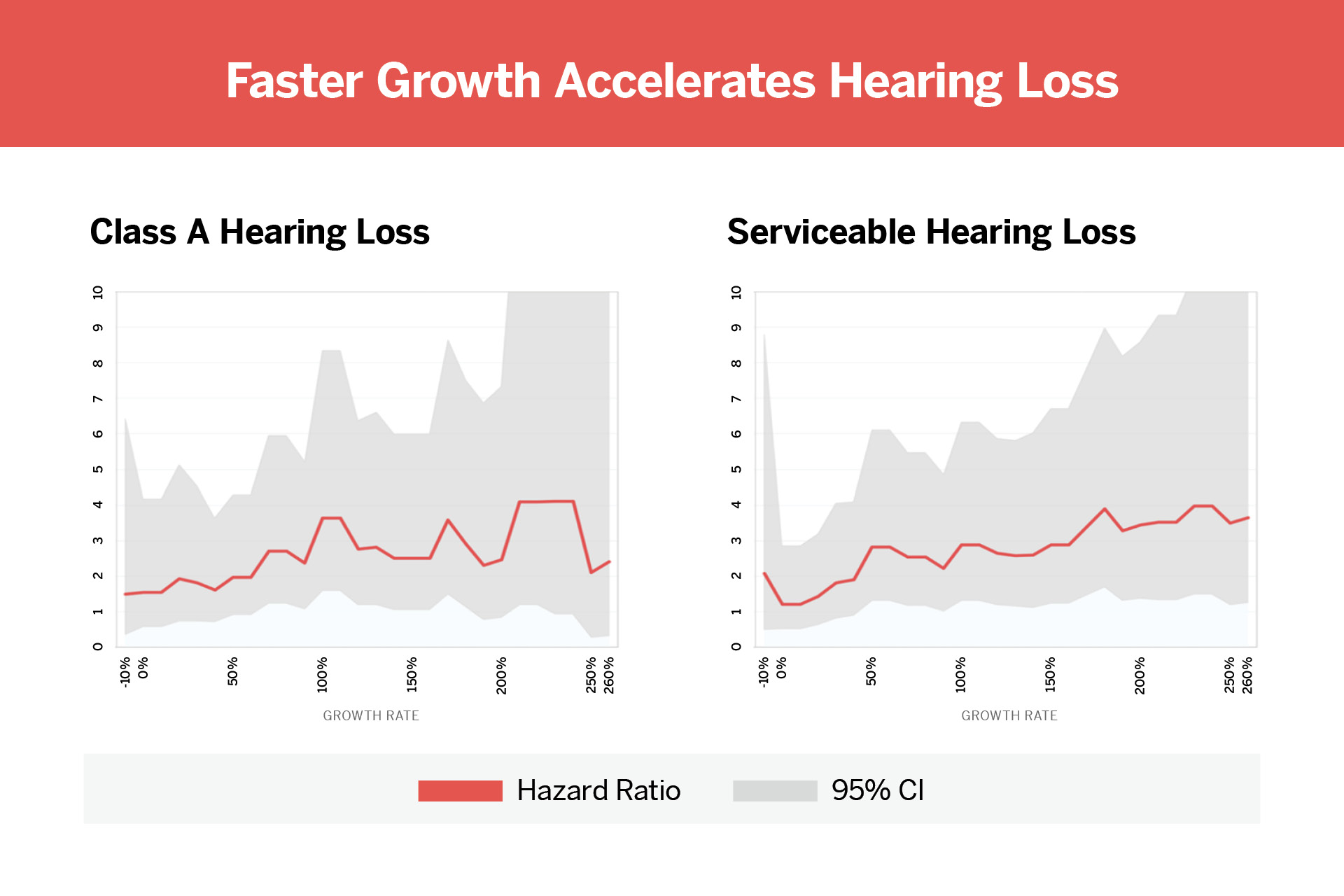
The average baseline tumor volume was 0.24 cubic centimeters. Participants with larger initial tumors experienced more hearing loss over time. The same was true for those with faster-growing tumors.
For every cubic centimeter increase, the researchers found an elevated risk of Class A hearing loss (hazard ratio=1.5) and serviceable hearing loss (hazard ratio=1.3). Risk appeared to increase linearly without any evident threshold growth rate resulting in a significant jump.
As a next step, the team plans to analyze how other factors, such as cochlear injury, nerve compression, tumor location, or neurodegeneration, might impact hearing loss in vestibular schwannomas. “The NYU Skull Base Surgery team has tremendous patient volumes. This data as well as previous work related to patient treatment outcomes helps us inform recommendations that assist patients with acoustic neuroma management decisions,” Dr. Roland says.