The Root Cause of a Months-Long Illness
A 19-year-old male with a congenitally diagnosed bicuspid aortic valve presented to the pediatric emergency department at NYU Langone Hospital—Long Island with a 5-month history of fatigue, intermittent cough and fever, rashes, weight loss, and migrating joint pain.
During the five weeks prior to arriving at NYU Langone and being referred to pediatric cardiologists Donna J. Better, MD, and Tasneem F. Hoque, MD, specialists with Hassenfeld Children’s Hospital, he developed night sweats, and his fevers became daily and continuous.
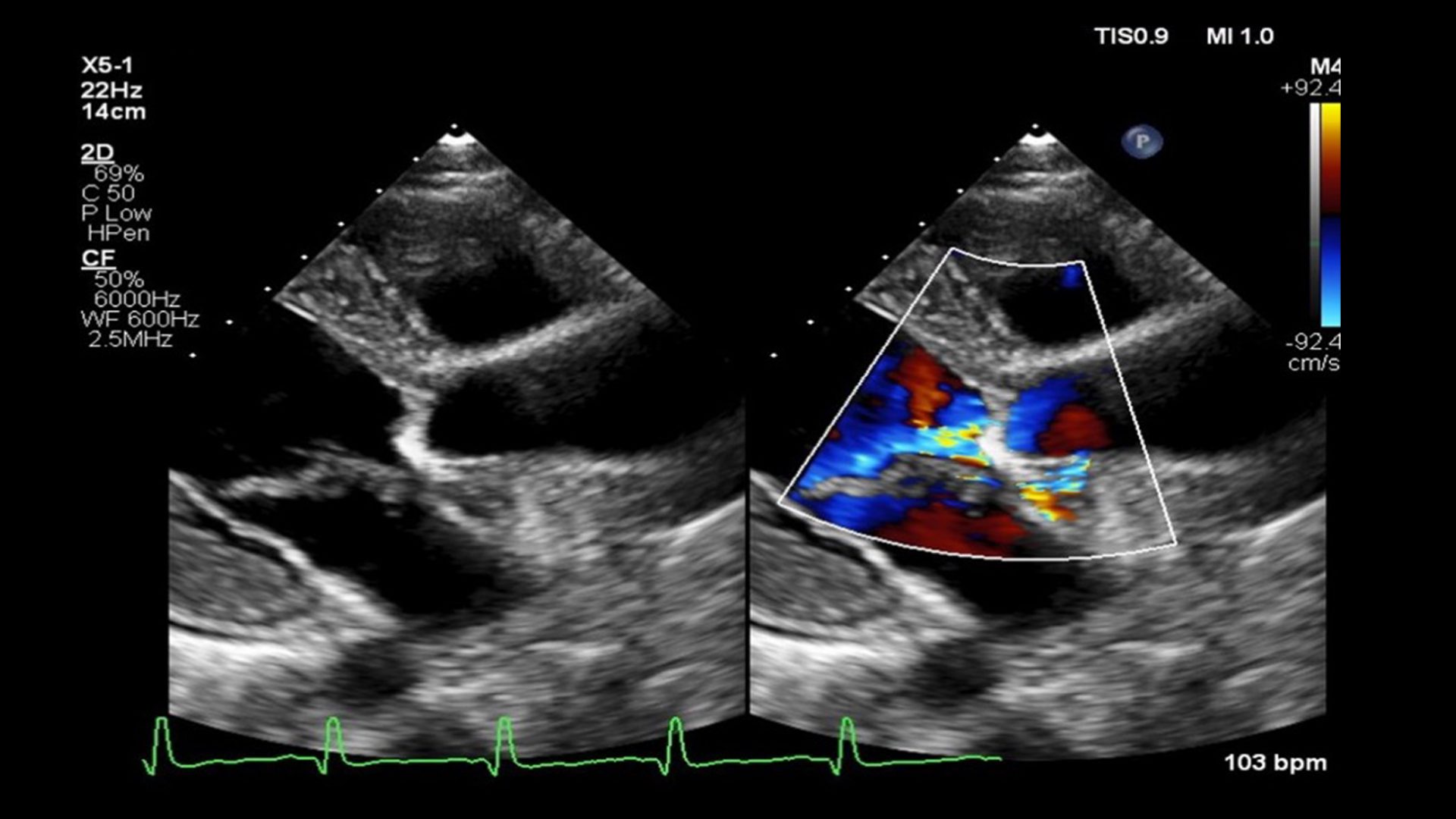
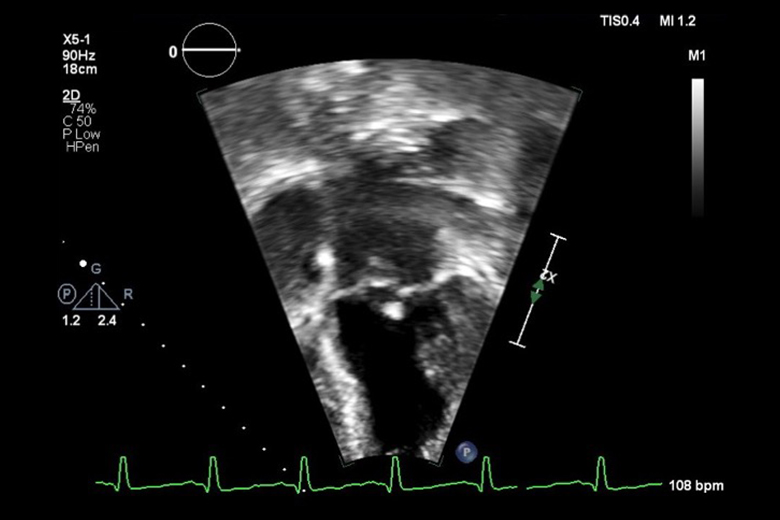
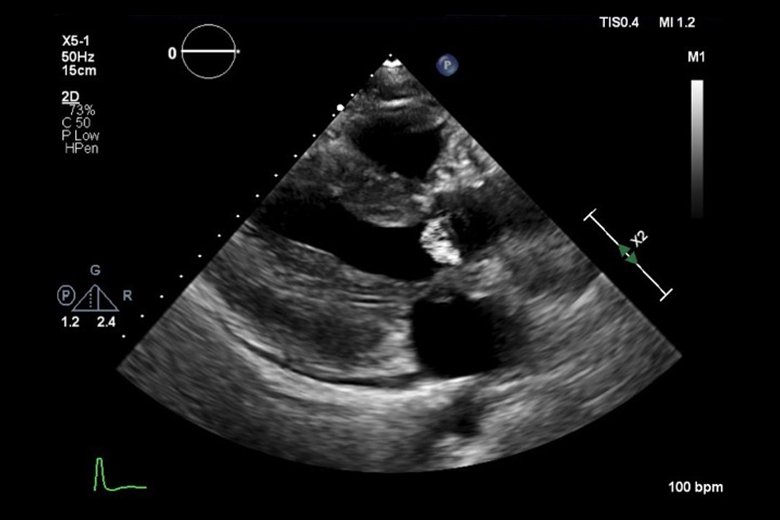
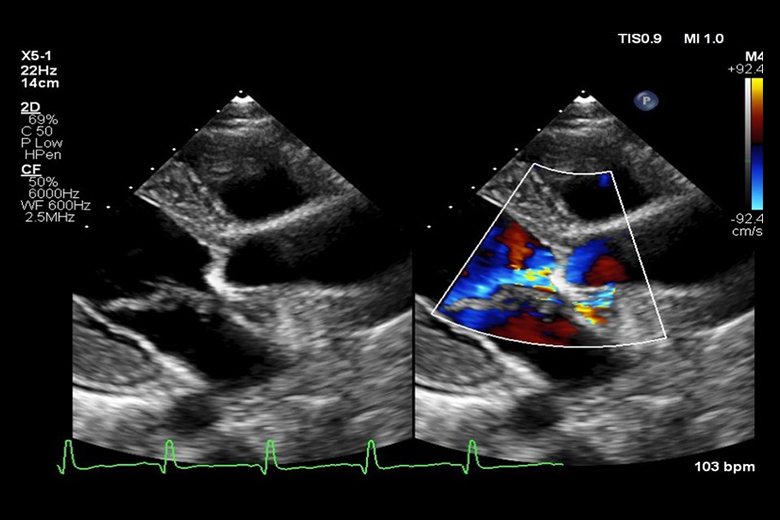
After an initial transthoracic echocardiogram revealed multiple vegetations and blood cultures were positive for Streptococcus mutans, they established a working diagnosis of infective endocarditis (IE). A follow-up MRA of the brain showed multiple small septic emboli.
“In patients with a known history of valve malformations and these symptoms, clinicians must maintain a high clinical index of suspicion for IE.”
Donna J. Better, MD
“Before coming to us, the patient had previously been seen by a pediatric cardiologist at another institution who did not consider the diagnosis of IE,” Dr. Better says. “In patients with a known history of valve malformations and these symptoms, clinicians must maintain a high clinical index of suspicion for IE to prevent morbidity and mortality.”
Because of concern for potential deterioration and need for cardiothoracic surgical intervention, the patient was transferred to NYU Langone’s Adult Congenital Heart Disease Program and put under the care of cardiothoracic surgeon T.K. Susheel Kumar, MD, and cardiologist Dan G. Halpern, MD.
“The strong and seamless collaboration and communication between our pediatric and adult congenital heart programs saved this patient’s life.”
T.K. Susheel Kumar, MD
Transesophageal echocardiography confirmed vegetations on both the aortic and mitral valves, while further imaging of the abdomen ordered secondary to abdominal pain revealed a splenic abscess.
Given extensive involvement of the aortic valve that resulted in both stenosis and severe regurgitation, the decision was made to replace the aortic valve using the patient’s own pulmonary valve, also called the Ross procedure.
“We first elected to perform laparoscopic splenectomy to reduce the burden of disease and risk of reinfection before proceeding with the Ross operation,” Dr. Kumar says. “The strong and seamless collaboration and communication between our pediatric and adult congenital heart programs saved this patient’s life.”
“Within a few days of surgery, the patient was back to normal activities. Follow-up echocardiograms revealed a perfectly functioning aortic valve,” Dr. Kumar says.