Over the past two decades, transcranial direct current stimulation (tDCS) has emerged as a promising therapy for a wide range of neurologic and neuropsychiatric disorders. Yet while specific tDCS products have been approved for such applications in the European Union and elsewhere, the method remains investigational in the United States.
Because tDCS can be effective in treating symptoms that resist conventional therapies, while posing little risk of serious adverse effects, many patients are eager to try it. One obstacle to widespread adoption, however, is the need to undergo daily sessions at a qualified facility. NYU Langone Health offers a novel alternative: the nation’s first remotely administered tDCS Program, led by Leigh E. Charvet, PhD.
Here, Dr. Charvet discusses tDCS’s expanding use cases and the program’s unique approach.
A Winning Combination
Physician Focus: Dr. Charvet, what led you to establish NYU Langone’s home-based tDCS Program?
Dr. Charvet: I was an early adopter of telerehabilitation approaches—using technology to provide therapies to people at home to help reduce their symptom burden and improve their quality of life. After leading a large home-based trial demonstrating the benefits of an online “brain training” program to treat cognitive impairment in patients with multiple sclerosis (MS), I was convinced of how much demand there is for telehealth solutions.
At the same time, exciting advances were occurring in the use of noninvasive brain stimulation technologies, including the safe and portable method of tDCS.
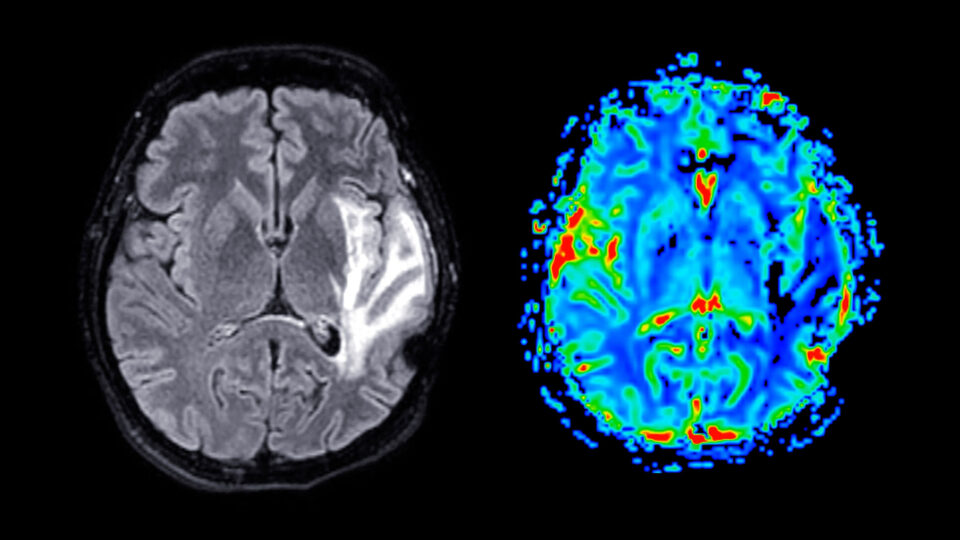
One use of tDCS is to direct the current to the region of the brain that is engaged in a training activity. A growing body of evidence shows that this method, known as “functional targeting,” can boost and harness the outcomes of other therapies. Imaging studies suggest it works by increasing cerebral blood flow in key areas and strengthening neuroplasticity.
That led me to investigate whether we could add tDCS to the home-based cognitive training program that we had studied.
My colleagues and I partnered with a tDCS device manufacturer, incorporating input from our patient participants, to develop a customized tDCS setup for home-based use. This includes specialized headgear and sponge electrodes, and fail-safe devices programmed to deliver a single dose of tDCS only after the patient has received clearance. We combined this technology with video visits and called the protocol “remotely supervised” tDCS (RS-tDCS).
“We’ve provided RS-tDCS to more than 200 patients from across the country with a wide range of chronic, progressive, and treatment-resistant conditions.”
Leigh E. Charvet, PhD
We then began a series of large trials studying the use of RS-tDCS for improving functional outcomes in cognitive and motor exercise programs. We first tested the technology in people living with MS, and have since expanded its use to people living with many different types of neurologic and psychiatric conditions.
Many patients sought to continue their tDCS treatment after participating in these studies. Patients with other disorders, some of them from outside New York State, began asking us if they could try a similar approach. And in 2019, we launched a program designed to do just that.
A Growing Roster of Use Cases
Physician Focus: Besides MS, what disorders does the program treat?
Dr. Charvet: We’ve provided RS-tDCS to more than 200 patients from across the country with a wide range of chronic, progressive, and treatment-resistant conditions—including recovery and preservation of function in dementias, post-stroke sequelae, traumatic brain injury, cerebellar ataxia, and Parkinson’s disease, as well as adjunctive support for patients in minimally conscious states, and symptom management in depression and headache.
Since early in the pandemic, we’ve also been treating patients with long COVID, which has shown encouraging results. That effort earned NYU Langone a lead role in the NIH’s ongoing RECOVER NEURO trial. And we’re about to publish a study showing improved language functioning in patients with primary progressive aphasia.
The Advantages of Home-Based Care
Physician Focus: How does NYU Langone administer tDCS remotely?
Dr. Charvet: We start with an intake call via telehealth to evaluate the patient’s needs. Then we have a group meeting, which includes everyone from medical staff to biomedical engineers, to design a customized treatment plan. We recommend an initial cycle of at least 20 half-hour sessions for patients and their clinicians to assess whether the therapy is having the desired effect.
“We’ve seen this therapy have profound impacts on patients with terrible conditions who have few other effective options for improving their symptoms.”
Treatment is delivered through Epic video visits, ensuring data security and integration with electronic health records. After receiving tDCS headsets targeting brain regions involved in their condition, patients work one-on-one with clinicians who are certified through our rigorous training process, which we also offer to labs nationwide that are studying this kind of approach.
We always pair tDCS with another therapeutic activity—anything from cognitive, physical, or language exercises for recovery from a neurologic condition to mindfulness meditation for the treatment of depression. The available evidence robustly supports tDCS as a supplement to such activities, rather than as a substitute for them.
Physician Focus: Wouldn’t it be simpler to just have patients come into a treatment center?
Dr. Charvet: It might be simpler for the clinicians, but home-based care offers two big advantages to patients. First, it’s accessible to people who aren’t willing or able to commute to a clinic five days a week. Second, remote administration allows us to provide tDCS to folks who don’t live near a facility that offers it.
We’ve seen this therapy have profound impacts on patients with terrible conditions who have few other effective options for improving their symptoms. These people are in such need of hope and help. We want to make sure they can get it.