Prototype implantable devices are moving into development, with the potential to fill major knowledge gaps in epilepsy research by offering real-time, state-of-the-art seizure monitoring.
Nearly one-third of patients living with epilepsy experience persistent, intractable seizures that do not respond to medication. The new technology could peel back the curtain about why this occurs.
“We now have the opportunity to build a new, ultrathin implantable device that can have thousands of measurement contacts instead of dozens,” says professor Daniel Friedman, MD, co-director of the video electroencephalogram laboratory and member of the Comprehensive Epilepsy Center.
Prototype Successes
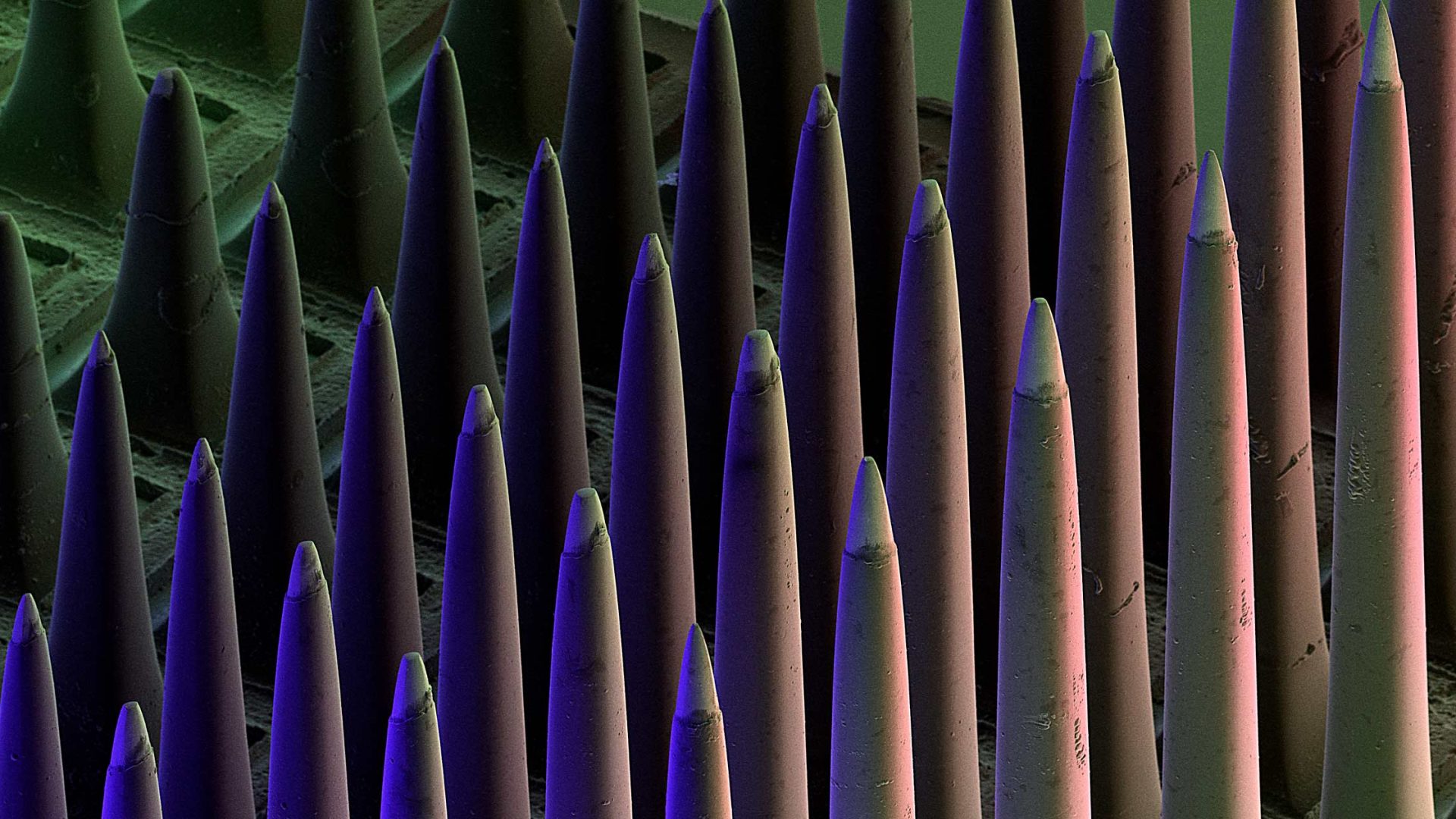
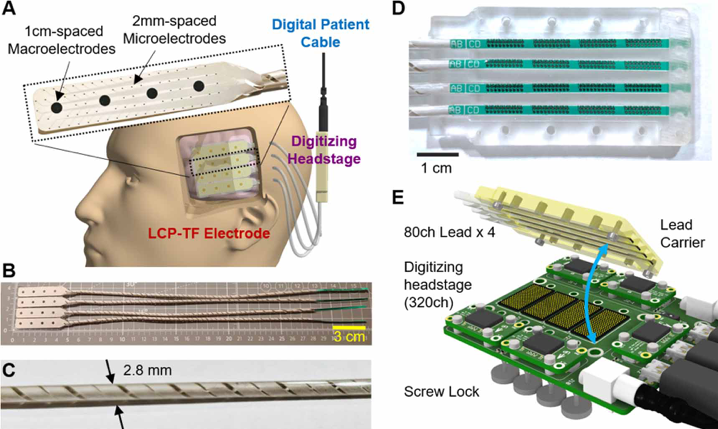
The implant—a flexible, liquid crystal polymer surrounding hundreds of thousands of electrodes—was developed via an expansive public-private partnership that recently earned $8 million from the NIH’s Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative. The funding will be shared between NYU’s Center for Neural Science, Duke University, the University of Utah, and Blackrock Neurotech.
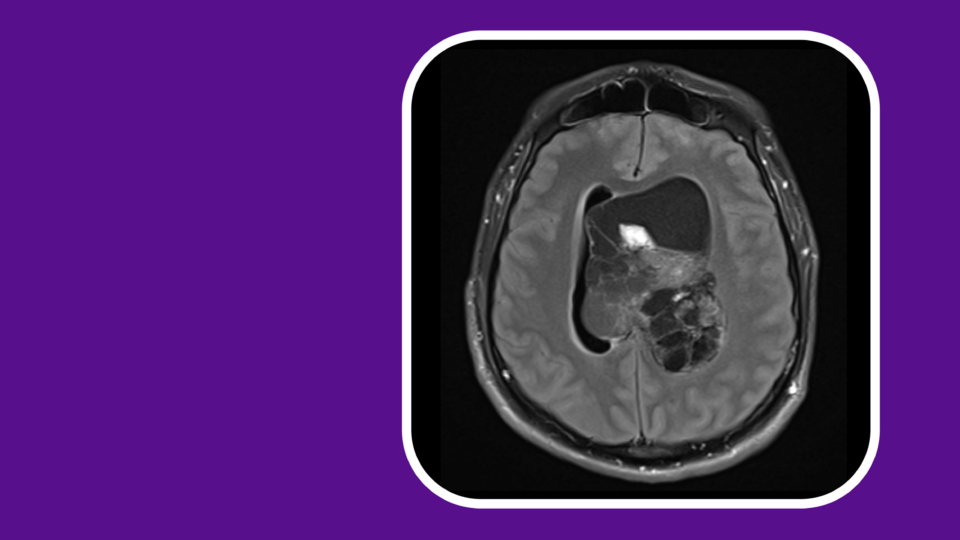
The collaborative team has already developed and tested several prototypes capable of collecting neural data directly before, during, and after seizures.
Their most recent iteration was successfully implanted and tested intraoperatively for up to 30 minutes in dozens of patients across the institutions. The researchers report their brain-machine interface achieves “25× higher electrode density, 20× higher channel count, and 11× reduced stiffness than conventional clinical electrodes.”
Further Development, Plus a Clinic Trial
With the new NIH support, the team will develop a further refined version of the device that can be implanted for up to 30 days. They anticipate the device will enable high-density sampling across multiple brain regions. A phase I clinical trial will follow initial testing, during which Dr. Friedman will serve as a site principal investigator.
The overarching goal is to capture a high-definition picture of brain microsignals that occur moments before epileptic seizures. Such data have been previously unobtainable, and are a critical step toward neurostimulative therapies designed to prevent debilitating seizures in patients with epilepsy.
Says Dr. Friedman, “Current technology used to capture brain activity related to epileptic seizure is decades old, and has limited our progress in developing new treatments.”
“Current technology used to capture brain activity related to epileptic seizure is decades old, and has limited our progress in developing new treatments.”
Daniel Friedman, MD
A Gateway to New Therapies
Indeed, neurostimulation as a potential treatment for neurologic conditions emerged in the 1980s. Since then, treatment options have vastly expanded to include laser ablation, precision surgeries, catheter-based interventions, and more.
Similarly, implantable tech has evolved to offer unprecedented benefits. Patients can now control computer systems and even prosthetic devices simply by thinking, Dr. Friedman says.
Previous research by Dr. Friedman and others has shown the promise of advanced seizure treatments made possible through implantable devices, including vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation.
Data from the implantable devices could open the door for more personalized interventions using these and other modalities for patients with epilepsy. More broadly, the devices could provide critical data to understand exactly why their seizures occur in the first place.