Chronic pain impacts up to one-third of children and adolescents worldwide, but remains underdiagnosed and undertreated. This is due in part to an insufficient understanding of the root causes of pain and a shortage of interdisciplinary teams specializing in its treatment.
Double board-certified in pediatric rehabilitation medicine and pain management, Jinpu Li, MD, NYU Langone Health’s director of pediatric chronic pain rehabilitation, prioritizes a multipronged approach to pediatric pain. Here, he explains his approach and the importance of integrated care in effectively managing chronic pain in young patients.
Physician Focus: Dr. Li, you emphasize education as a central element of your approach to chronic pain treatment. Can you expand on that?
Dr. Li: By the time I see many of my patients, they have seen multiple specialists in other fields. And I’ve found that one of the most important things I give my patients as we begin their treatment is the simple acknowledgment that their pain exists and is very real. So I start by explaining the pathophysiological basis of pain.
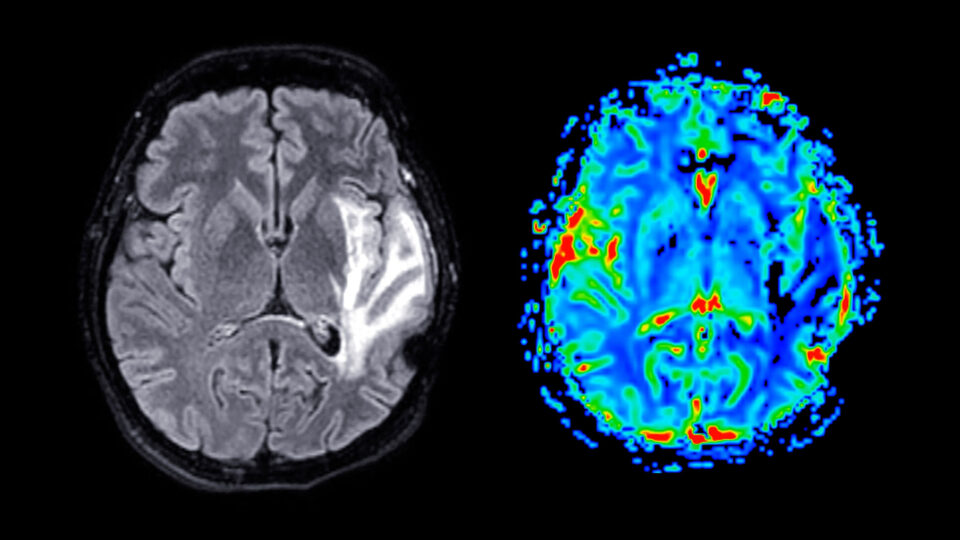
“I use the analogy of ‘camera’ and ‘snapshot.’ The brain acts as the camera; when tissue is injured, a signal is sent to the brain, which takes a snapshot and stores the image, registering it as pain.”
Jinpu Li, MD
I use the analogy of “camera” and “snapshot.” The brain acts as the camera; when tissue is injured, a signal is sent to the brain, which takes a snapshot and stores the image, registering it as pain. Normally, once the tissue heals, the brain deletes the snapshot, resolving the pain. But for some people, due to various reasons, the brain holds on to the snapshot and does not delete it, causing ongoing pain despite there being no tissue injury. Additionally, sometimes the brain is hypersensitive, taking snapshots of normal physiological functions, leading to pain perception without any actual injury.
Many patients feel relieved after hearing this. They feel heard and understood. This is the first step of healing.
Physician Focus: What types of conditions do children typically present with in your practice?
Dr. Li: We see children and adolescents with a wide variety of pain-associated conditions, including musculoskeletal and spinal pain, chronic postsurgical and post-trauma pain, chronic secondary visceral pain, chronic neuropathic pain, and chronic headache and orofacial pain. Examples of these conditions are chronic pain related to sports injuries, herniated disc, facet-mediated back pain, neuropathic pain related to nerve injuries, and pain associated with joint hypermobility.
We also frequently see primary pain disorders, in which the pain is not caused by an underlying disease or injury. Examples include complex regional pain syndrome (CRPS) and amplified musculoskeletal pain syndrome (AMPS), which is similar to fibromyalgia and involves heightened pain perception.
Physician Focus: What is your general approach to treating these patients?
Dr. Li: Our approach is team-oriented and highly tailored to meet the needs of each patient and their family.
We begin with a thorough intake appointment that assesses the patient’s complete medical history, psychological comorbidities, and functional status. We also consider the family’s history and explore how the patient’s pain may result from—or contribute to—certain family dynamics. Working closely with physical therapists, occupational therapists, social workers, and other specialists, we develop a comprehensive treatment plan that aligns with the patient’s and family’s specific needs and goals.
“We also consider the family’s history and explore how the patient’s pain may result from—or contribute to—certain family dynamics.”
The treatment plan typically includes a combination of medical interventions—such as oral medications, various muscle, joint and spinal injections, imaging-guided nerve blocks, and minimally invasive surgical procedures like implantable neuromodulation devices—alongside physical and occupational therapies and pain psychology.
Physician Focus: Can you tell us more about how pain psychology plays a role in your team approach to patient care?
Dr. Li: Pain management truly integrates both body and mind, as psychological factors can both contribute to and result from pain. For instance, a child with a history of abuse is at high risk for developing chronic pain. And children who live with pain often then have concomitant diagnoses of anxiety or depression. The anticipation of pain can lead to avoidant and maladaptive behaviors, as the child wants to do anything to avoid the onset of pain.
This is why we collaborate closely with psychologists and social workers. They treat the entire family, providing cognitive–behavioral techniques to help children improve their coping skills, along with mindfulness practices and other support for parents and family members.
Physician Focus: What are some of the latest advancements in pain medicine that you might incorporate into a care plan?
Dr. Li: One of the exciting advancements in pain management is the emergence of neuromodulation. I am closely following the research on using transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) in managing chronic pain. We started using neuromodulation techniques like peripheral nerve stimulation and spinal cord stimulation for certain cases of refractory chronic pain in adolescents.
“I think it’s a strength that in our field of pain rehabilitation, we’re focused on improving function, not simply reducing pain.”
Importantly, pain management often requires trying several treatment approaches to find what works. For instance, for the past year, I have followed a patient who presented with erythromelalgia, which causes pain and burning in the lower extremities. The patient was experiencing frequent emergency room visits and hospital admissions for pain crises. After attempting a combination of medications and periodic nerve block treatments without significant improvement, we implanted a neuromodulation device, a peripheral nerve stimulator, which has meaningfully reduced his pain. His pain still fluctuates, but we were able to keep him out of the emergency room for the past 10 months.
Physician Focus: Finally, what inspired you to specialize in both pain management and pediatric rehabilitation medicine?
Dr. Li: My interest stemmed from observing the profound impact pain has on a patient’s function and quality of life during my pediatric rehabilitation medicine training. We see many patients who suffer from chronic pain, which profoundly impacts their overall wellbeing, both physically and emotionally. I think it’s a strength that in our field of pain rehabilitation, we’re focused on improving function, not simply reducing pain.