Referral Notes:
- To minimize the risk of type 3c diabetes after pancreatectomy, NYU Langone’s Total Pancreatectomy with Islet Autotransplantation program reinfuses a patient’s islet cells in the liver.
- NYU Langone is one of the few centers to perform pancreatic islet harvesting and processing right in the OR, maximizing islet survival prior to reinfusion.
- Primarily for patients undergoing pancreatectomy for painful chronic pancreatitis, the program is exploring expanded indications.
For patients that require a total pancreatectomy for chronic pancreatitis or other conditions, loss of the pancreas and its ability to make insulin and other blood sugar-regulating hormones like glucagon can lead to type 3c diabetes. “These patients have a problematic and unpredictable response to insulin; it can be very hard to manage and they can have life-threatening hypoglycemic events,” says Katherine A. Morgan, MD, a hepatobiliary and pancreatic surgeon at NYU Langone Health.
A unique approach within NYU Langone’s Total Pancreatectomy with Islet Autotransplantation (TPIAT) program, led by Dr. Morgan and launched in August 2025, aims to minimize the risk of postoperative diabetes. The approach involves harvesting pancreatic islets directly in the operating room (OR) so they can be immediately reinfused. “There’s no delay and it minimizes islet loss by allowing us to immediately process and infuse them,” Dr. Morgan says.
The health system is one of the few in the New York region with a dedicated interest in pancreatitis and among the few worldwide with expertise in islet autotransplantation.
An Immediate Harvest
At NYU Langone, a total pancreatectomy initially proceeds just as it would for an organ transplant. “We preserve the blood flow until the last minute and then immediately flush the pancreas, prep it, and put it in a cold solution to preserve the islets before we start the process of harvesting them,” Dr. Morgan says.
“The more islets we’re able to harvest and autotransplant back into the patient, the higher the chances are that they’ll be insulin-free after surgery.”
Katherine A. Morgan, MD
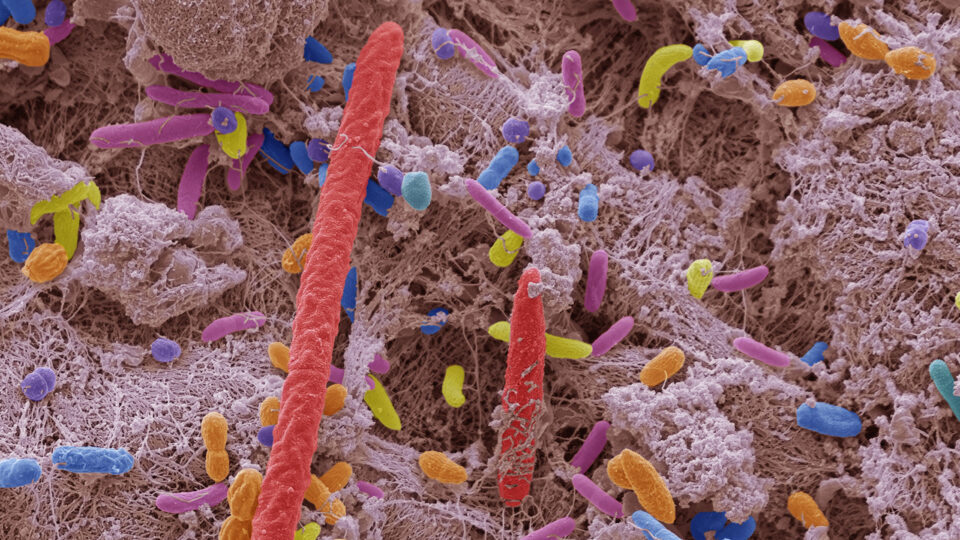
Many medical centers take the resected pancreas to a separate lab or institution to harvest the cells, leading to a considerable lag time before the cells are reinfused back into the patient. At NYU Langone, the harvesting process for the resected pancreas begins immediately in the OR, which contains an islet isolating machine. The process mechanically and enzymatically digests the pancreas, leaving islet cell clusters that can be separated from the organ’s ductal and connective tissues.
A centrifuge separates out and concentrates the islet cells by mass. “We’re able to take that pellet of islets and put it into a solution of albumin along with an antibiotic and blood thinner, and then put it back into the patient,” Dr. Morgan says. “The more islets we’re able to harvest and autotransplant back into the patient, the higher the chances are that they’ll be insulin-free after surgery.”
Reinfusion in the Liver
The most common infusion route for the islet solution is through the patient’s portal vein into the liver, where the cells disperse. Because the islet cells normally encounter blood from the gastrointestinal tract, Dr. Morgan says, the liver’s blood supply offers the best alternative for regulating blood sugar.
“From a lot of work in the lab trying to get islets to grow, we know that they like to have a scaffolding or structure to grow on, and the liver is an ideal structure for that,” Dr. Morgan says.
“It’s a pretty amazing process. We see them start to make their own insulin within a few days.”
Over the first few weeks, surviving cells develop their own blood supply and re-form normal islet clusters. “It’s a pretty amazing process,” she says. “We see them start to make their own insulin within a few days, and they get better at making it over the first few months after surgery.”
One main focus of the program is maximizing the survival of autotransplanted islet cells. “Our dream down the road is to reliably grow islets for patients,” Dr. Morgan says.
In the meantime, the program is continuing to push the envelope by pursuing new collaborations and delving into more applications beyond pancreatitis. “That’s also what makes our program unique: we’re looking into these extended indications for islet autotransplantation, such as after surgery for benign or low-grade pancreatic tumors or even pancreatic cancer,” she says.