A growing body of evidence suggests that atherosclerotic-related inflammation may play a role in the pathogenesis of inflammatory bowel disease (IBD). Yet to date, there has been little research assessing the relationship between a diagnosis of an atherosclerotic-related condition and the risk of eventually developing IBD.
In a study presented at Digestive Disease Week 2023, researchers led by gastroenterologist Adam Faye, MD, an assistant professor of medicine and population health at NYU Langone Health, explored that question in unprecedented scope and detail.
“That the association shows up long before diagnosis suggests we’re not just seeing two conditions that happen to co-occur.”
Adam Faye, MD
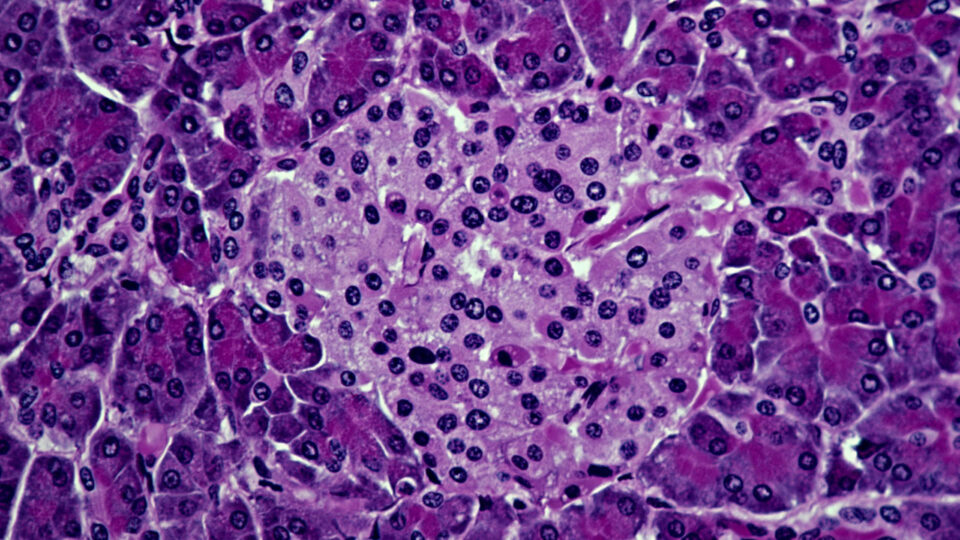
Using the Swedish Patient Register and the ESPRESSO (Epidemiology Strengthened by histoPathology Reports in Sweden) cohort, the team identified more than 56,000 individuals with IBD between 2002 and 2021, and matched these cases to over 530,000 controls. They then calculated odds ratios (OR) for exposure to an atherosclerotic-related condition (myocardial infarction, thromboembolic stroke, or atherosclerosis itself) before diagnosis with IBD.
“The Swedish data is one of the best assets available for this type of research,” Dr. Faye explains, “because it enables us to track diagnoses, healthcare usage, pathology reports, and prescriptions for every patient in the country over decades, with almost no loss to follow-up.”
An Unprecedented Investigation
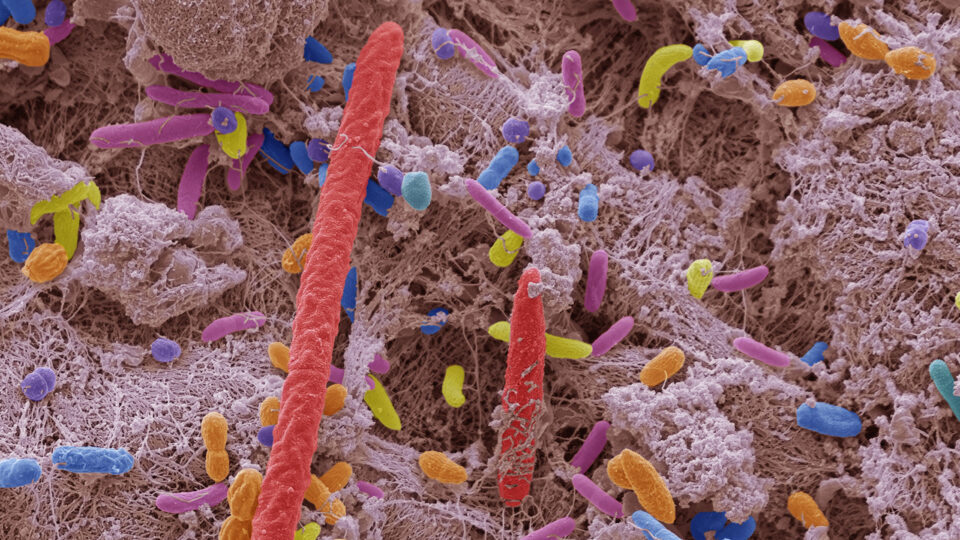
It has long been known that IBD and atherosclerosis have partly overlapping pathophysiology, with plaque deposition leading to immune activation and upregulation of pro-inflammatory cytokines.
A 2013 study found the risk for ischemic heart disease to be highest in the year following a diagnosis of IBD, suggesting that atherosclerosis may have long preceded symptomatic bowel inflammation. More recently, studies have shown that statin use, which reduces the inflammatory burden associated with atherosclerosis, may reduce the risk of IBD.
The new investigation, however, was the first population-based case-control study to examine the potential links between atherosclerosis and the development of IBD.
Dr. Faye and his colleagues evaluated the epidemiological associations between a prior atherosclerotic condition and the development of IBD, as well as between the number and types of atherosclerotic conditions and the development of IBD.
An Array of Associations
The team found that older adults who developed IBD were significantly more likely to have an atherosclerotic-related condition as compared to both the general population and sibling controls. Results were statistically significant for both Crohn’s disease and ulcerative colitis and were consistent regardless of the patient’s age at IBD diagnosis.
“Atherosclerosis prevention may be important not only to limit the development of cardiovascular disease, but also to limit the development of IBD.”
The highest odds of a preceding atherosclerotic condition were seen in the 12 months before the IBD diagnosis, with patients with IBD being 78 percent more likely to have experienced an atherosclerotic condition within the year preceding their diagnosis compared to controls. But odds were also increased even five or more years earlier.
“The fact that the association shows up long before diagnosis suggests we’re not just seeing two conditions that happen to co-occur,” says Dr. Faye.
All types of atherosclerotic conditions were associated with increased odds of IBD, though the highest was for atherosclerosis itself—possibly, the researchers hypothesize, because patients with myocardial infarction or stroke were less likely to survive long enough to develop IBD.
In addition, the odds for developing IBD were higher when two or more atherosclerotic conditions were present.
“Our findings suggest that atherosclerosis prevention may be important not only to limit the development of cardiovascular disease, but also to limit the overall inflammatory burden and development of IBD,” says Dr. Faye.
Although further research will be required to clarify the associations between the two conditions, he adds, these results might point toward future interventions (such as prophylactic statin administration) for patients with known risk factors for IBD.
Disclosures
Dr. Faye has received consulting honoraria from Bristol Myers Squibb.