A first-of-its-kind clinical trial is testing whether an implanted stimulatory device might aid human patients with treatment-refractory rheumatoid arthritis.
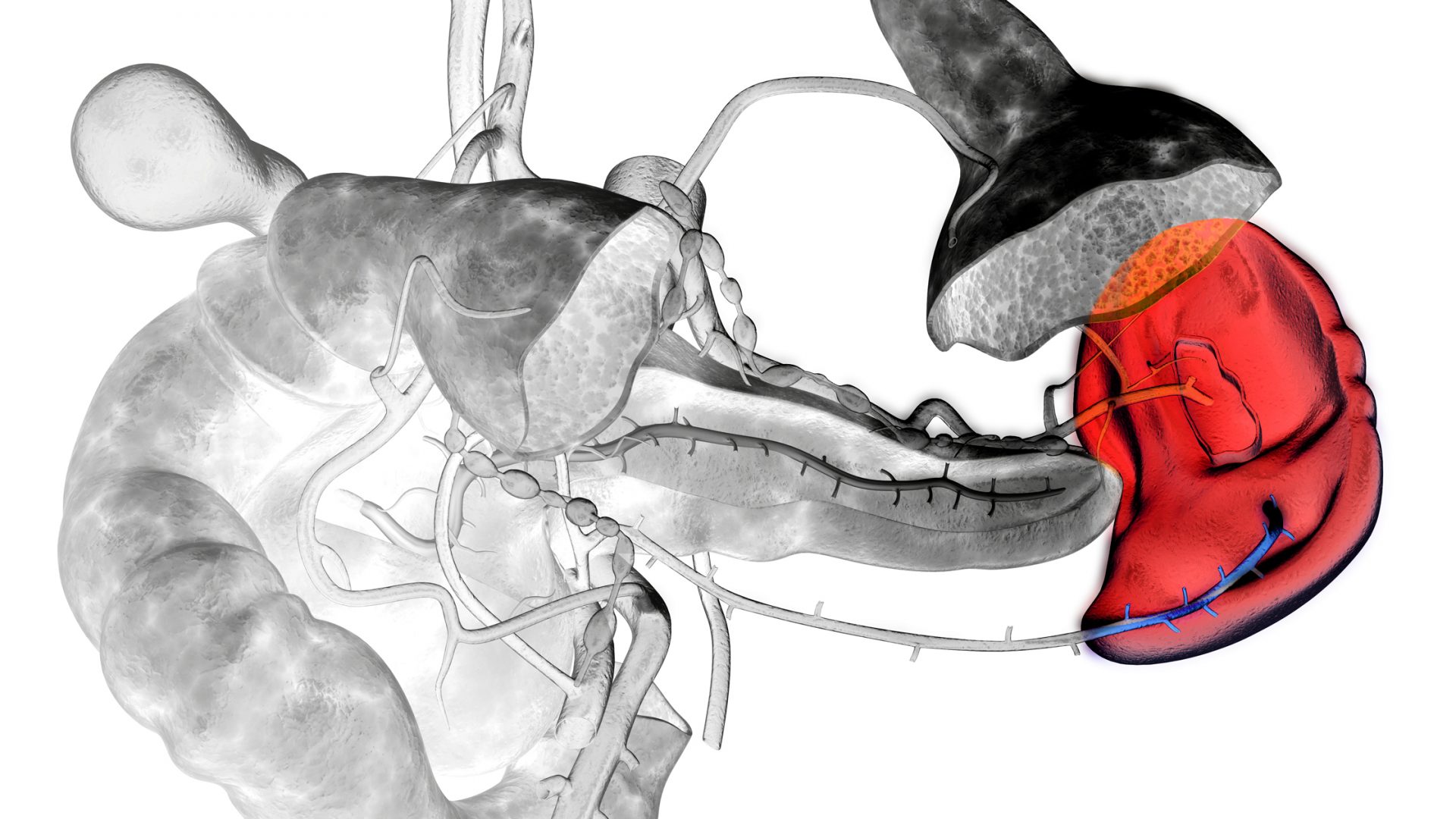
In animal models of inflammation, repeated stimulation of the splenic nerve, a branch of the vagus nerve, can change lymphocyte trafficking and the inflammatory response. The human clinical trial is seeking to do the same by propagating nerve signals that shift circulating immune cells from a pro-inflammation to an inflammation-resolving state.
The key-sized device, developed by Galvani Bioelectronics, emits pulses of electricity to the splenic nerve to stimulate the immune system. NYU Langone Health researchers partnered with the company to help design the randomized, double-blind trial and to serve as a lead center. In January 2022, David H. Goddard, MD, a clinical professor in rheumatology, collaborated with bariatric surgeons Megan Jenkins, MD, and Loic S. Tchokouani, MD, to implant the device in the first North American patient—and just the second worldwide.
The Splenic Nerve: A Promising Target
“One of the hallmarks of rheumatoid arthritis is an overactivity of B lymphocyte function,” Dr. Goddard says. “That’s one of the reasons why you see very high levels of immunoglobulin being produced at the same time.”
Damping down that immune cell activity may help shut down the cascade of downstream effects such as the local production of inflammatory mediators like tumor necrosis factor and cytokines within the synovial membrane of a joint.
“There’s quite a bit of medical literature suggesting that stimulation of different parts of the autonomic nervous system can result in significant changes in bodily function. It’s also been clear over a long period of time that if you stimulate the vagus nerve, you can affect the way in which lymphocytes not only traffic but also behave.” For rheumatoid arthritis, reprogrammed immune cells that travel to the synovium may help reduce or resolve inflammation and pain in the affected joints.
A Potential Key to Modulating Immune Cells
The experimental neurostimulator, which wraps around the splenic nerve, is connected via a cable to a second device that sits in a pouch created in the patient’s anterior abdominal wall. That device, in turn, is connected by Bluetooth to an external controller that turns the device on for a defined period of nerve stimulation every day.
Although stimulating a main trunk of the vagus nerve can bring unwanted effects such as a drop in blood pressure, stimulating nerve function close to the spleen may affect lymphocytes without the untoward effects of vagal nerve stimulation.
The trial is actively enrolling patients and seeking referrals. Altogether, the multicenter trial is aiming to enroll 26 patients. After the device or a sham used as a placebo has been implanted in the first four participants, Dr. Goddard says, the FDA will review the trial data. “There’s a lot of excitement around the fact that we’ve managed to get this far. Now the next question is, how effective is it really in humans?”
“There’s a lot of excitement around the fact that we’ve managed to get this far. Now the question is, how effective is it really in humans.”
David H. Goddard, MD
The therapy could have enormous potential not only for rheumatoid arthritis, but also for a range of other autoimmune diseases including inflammatory arthritis and inflammatory muscle diseases if proven effective, Dr. Goddard says.