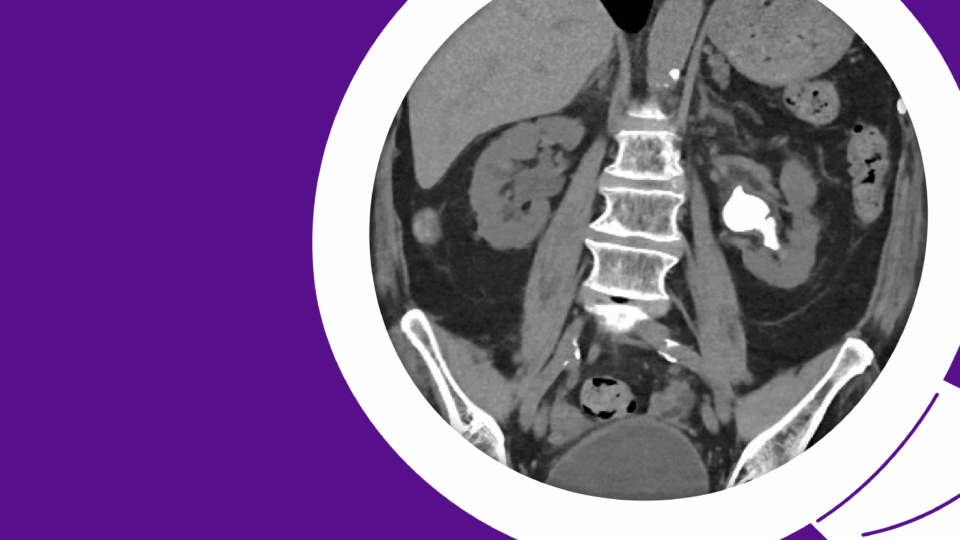
A 57-year-old male presented with a history of treated thyroid cancer and lower urinary tract symptoms (LUTS). His international prostate symptom score (IPSS) was 25 and an upper tract ultrasound revealed a 160-gram prostate.
Some improvement in urinary symptoms was seen with tamsulosin and finasteride. However, the impact of treatment on sexual health was significant. Intermittent self-catheterization was also required for high postvoid residual volume, and the patient did not wish to continue this.
An office cystoscopy confirmed bladder outlet obstruction secondary to benign prostate hyperplasia (BPH), a common cause of LUTS, and the patient was counseled on surgical options. After considering GreenLight, transurethral resection of the prostate (TURP), anatomical endoscopic enucleation of the prostate (AEEP) with Holmium, Aquablation, and simple robotic prostatectomy, the patient elected for the Aquablation procedure.
The following Case of the Month illustrates how Aquablation safely and effectively treats a very large prostate size normally managed by simple prostatectomy or AEEP, but with lower rates of urinary incontinence and ejaculatory dysfunction.
The case also exemplifies why I consider Aquablation to be the Swiss Army knife of surgical therapies for BPH.
Case Highlights:
- Aquablation received de novo clearance from the FDA for the resection and removal of prostate tissue in males suffering from LUTS due to BPH.
- The technique is appropriate for all prostate sizes, including very large prostates >150 mL, and is adaptable to any type of bladder outlet obstruction.
- The technique significantly improves IPSS and surpasses all other BPH procedures in preserving ejaculatory function.
- In the case presented here, the patient reported an IPSS of 25 before treatment. After Aquablation, his IPSS dropped to 4, and he reported preserved erectile and ejaculatory function; his only medication was finasteride.
Patient Case
When the patient first presented to our care, he experienced nocturia three times per night, urinary frequency every two hours, urinary urgency, and a weak urinary stream. He achieved significant improvement in LUTS on tamsulosin but eventually went into acute urinary retention requiring Foley catheterization. At that time, an upper tract ultrasound confirmed the presence of two normal renal moieties, a normal-appearing bladder, and an enlarged prostate with a large median lobe.
He then increased tamsulosin to 0.8 mg daily, started finasteride, and subsequently voided spontaneously. However, high postvoid residuals required self-catheterization four times daily.
An office cystoscopy was completed, confirming a normal anterior urethra and trilobar prostate hyperplasia. Urodynamic study was not performed due to his cystoscopic findings, prostate size, and lack of relevant comorbidities. Digital rectal exam demonstrated a large, smooth prostate. The PSA was 2.1 ng/dL.
The patient elected for Aquablation after being counseled on his surgical options. He did not wish to continue intermittent catheterization, did not tolerate the retrograde ejaculation of tamsulosin, and wished to preserve his erectile and ejaculatory function.
Aquablation: The Clinical Trials
Treatments of bladder outlet obstruction range from medical therapy to minimally invasive procedures to open surgery. The goal of surgical therapy is simply to reduce outlet resistance. However, techniques must be effective in symptom score reduction and durability and be associated with minimal peri- and postoperative complications. Other goals should be a short learning curve and minimal sexual dysfunction.
Among the newer, novel resective techniques is Aquablation therapy, delivered by the PROCEPT BioRobotics’ AquaBeam Robotic System. It has attracted attention as a minimally invasive technique that is as effective and safe as other resective treatments, but with minimal to no negative impact on erectile or ejaculatory function.
Aquablation employs a robotically controlled, room-temperature waterjet to remove obstructing prostate tissue1. The AquaBeam Robotic System received de novo clearance from the FDA in December 2017. It is indicated for the resection and removal of prostate tissue in males suffering from LUTS due to BPH.
The safety and efficacy of Aquablation therapy with the AquaBeam Robotic System have been rigorously investigated. The WATER study was a randomized, pivotal trial comparing Aquablation therapy against TURP. It showed that Aquablation provided the same durable outcomes and lower surgical retreatment rate as TURP at five years for prostate sizes 30 to 80 mL while maintaining a superior ejaculatory profile. The WATER study enrolled 181 patients ages 45 to 80 years with urinary symptoms due to BPH across 17 sites in the United States, the United Kingdom, Australia, and New Zealand, demonstrating superiority and noninferior primary efficacy results compared to TURP2. Other studies have demonstrated noninferiority and even superiority to TURP3,4.
The WATER II study enrolled 101 male patients with prostates 80 to 150 mL between the ages of 45 to 80 years with urinary symptoms due to BPH at 16 sites in the United States and Canada. The WATER II study demonstrated significant improvement in both symptom scores and urinary flow rates, with similar length of stay reported in the WATER study5.
A meta-analysis of four clinical trials (WATER, WATER II, OPEN WATER, and FRANCAIS WATER) with 425 patients (volumes 20 to 150 mL) and a one-year follow-up showed an average IPSS improvement of 16 points, 20.5 mL/second urinary peak flow rates, 3.3-point improvement in quality of life, 0 percent erectile dysfunction, 0.5 percent incontinence, and only a 10.8 percent incidence of ejaculatory dysfunction6.
Based on the above data and other sources, the American Urologic Association included Aquablation therapy in its 2019 Practice Guidelines for the “Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia”7. Today, Aquablation therapy provides a minimally invasive option in a field already populated by Optilume, iTIND, UroLift, Rezum, GreenLight, TURPs, AEEPs, and simple robotic or open simple prostatectomies. It has a short learning curve of about 10 to 20 cases and a high level of predictability and reproducibility8.
Aquablation: The Procedure
The patient’s Aquablation procedure was performed in the operating room under general anesthesia9. An SIUI Apogee 2300 biplane transrectal ultrasound was first inserted for optimal prostate imaging. The 24 Fr handpiece was then inserted transurethrally into the patient’s bladder and then mounted on the bed-mounted robotic articulating arm.
Using real-time prostate visualization and PROCEPT planning software on the CPU, the waterjet angles and a surgical contour were planned and the waterjet robotic ablation begun. As the waterjet moved from median lobe to prostate apex, adenomatous tissue was removed with a pendulum-like motion.
Once the jet reached the ejaculation safety zone, its pattern was converted to a “butterfly-cut” mode to avoid injury to the ejaculatory ducts on the prostatic urethral floor.
A second full pass was performed, and then the handpiece was removed. A 26-Fr resectoscope was inserted, clot evacuation was done, and focal bladder neck cauterization was performed. Minor resection of treated prostate tissue was resected and sent for pathology. Finally, a 24 Fr 3-way Coude catheter was inserted and the patient was observed on traction. Postoperative continuous bladder irrigation (CBI) was performed until the following day.
The patient was discharged on postoperative day one and passed a trial of void on postoperative day two with a postvoid residual of 120 mL. At a six-week follow-up, the patient had no complaints. He had a negative urine culture and an IPSS of 4. He had preserved erectile and ejaculatory function, and his only medication was finasteride.
Discussion
One of the three distinctive and attractive features of Aquablation is its versatility. Some procedures are only appropriate for certain types of prostate sizes or configurations. Aquablation has real potential to dominate the BPH minimally invasive therapy market because of its ability to be the Swiss Army knife of BPH surgical therapies. It can safely and effectively treat all prostate sizes (20 grams and up) and can also treat various forms of bladder outlet obstruction, including high-riding bladder necks, prostates with median lobes of any size, lateral lobe compression, very long prostates, prostate synechiae, and overhanging anterior prostate tissue. It is also safe and effective in patients with prior treatments, such as UroLift, Rezum, brachytherapy, and external beam radiation.
Another enticing feature is Aquablation’s ability to treat all prostate sizes. Until now, surgical management options for men with very large prostates (>150 mL) were limited to simple prostatectomy (open, laparoscopic, or robotic) and AEEP (Holmium and thulium). These surgical options are associated with increased surgical risks, such as increased operative time, risk of bleeding, transfusions, ejaculatory dysfunction, and a prolonged indwelling catheter time10. The proliferation of AEEP has been limited due to its steep learning curve and a relative paucity of training opportunities.
After earlier reports of bleeding in the WATER and WATER II trials, PROCEPT developed an optimal hemostasis technique of focal bladder neck cauterization that included removal of frondular ablated tissue at the bladder neck as well as any targeted focal cautery of any obvious arterial bleeding. In April 2021, a study of more than 2,000 patients undergoing this technique yielded a transfusion rate of 0.8 percent for treated prostates with volumes of 20 to 363 mL11. Further meta-analysis of the WATER, WATER II, and OPEN WATER trials report a composite transfusion rate of 0.1 percent12.
The other complication deserving of discussion is ejaculatory dysfunction. Aquablation preserves anterograde ejaculation rates in over 90 percent of men, better than any other resective BPH procedure. It is important to note that Aquablation is the only procedure where de novo ejaculatory dysfunction remained low despite larger prostate sizes (80 cc to 150 cc)13,14. This potential complication is getting more discussion time preoperatively, now that men and their partners are more educated about which treatments are associated with ejaculatory dysfunction and which ones are not. The days of treating urologists downplaying the importance of male orgasmic function in their patients are numbered as more men are understanding that retrograde ejaculation and anejaculation are often inferior in sensation to anterograde ejaculation.
Conclusion
Physicians counseling patients with obstructive BPH should be aware of Aquablation therapy as it is able to comparatively improve IPSS scores, has superior durability to TURP, has minimal complications, and is superior to other resective BPH procedures in preserving ejaculatory function.
Aquablation is adaptable to any type of bladder outlet obstruction and is appropriate for any prostate size. The learning curve is short, and operative times are consistent and reproducible.
References
1. Zorn et al. (2022). Aquablation treatment for benign prostate hyperplasia: Current standardized procedure. Journal of Endourology. DOI.
2. Oumedjbeur et al. (2023). Aquablation versus TURP: 5-year outcomes of the WATER randomized clinical trial for prostate volumes 50-80 mL. Canadian Journal of Urology. PubMed.
3. Plante et al. (2019). Symptom relief and anejaculation after aquablation of transurethral resection of the prostate: Subgroup analysis from a blinded randomized trial. BJU International. DOI.
4. Gilling et al. (2020). Three-year outcomes after Aquablation therapy compared to TURP: Results from a blinded randomized trial. Canadian Journal of Urology. PubMed.
5. Bhojani et al. (2023). Aquablation therapy in large prostates (80-150 mL) for lower urinary tract symptoms due to benign prostatic hyperplasia: Final WATER II 5-year clinical trial results. Journal of Urology. DOI.
6. Elterman et al. (2021). Meta-analysis with individual data of functional outcomes following Aquablation for lower urinary tract symptoms due to BPH in various prostate anatomies. BMJ Surgery, Interventions, & Health Technologies. DOI.
7. Dornbier et al. (2020). The new American Urological Association benign prostatic hyperplasia clinical guidelines: 2019 update. Current Urology Reports. DOI.
8. El Hajj et al. (2022). Learning curve in aquablation: An international multicenter study. World Journal of Urology. DOI.
9. MacRae et al. (2016). How I do it: Aquablation of the prostate using the AQUABEAM system. Canadian Journal of Urology. PubMed.
10. Nguyen et al. (2020). Operative time comparison of Aquablation, Greenlight PVP, ThuLEP, GreenLEP, and HoLEP. World Journal of Urology. DOI.
11. Elterman et al. (2021). Focal bladder neck cautery associated with low rate of post-Aquablation bleeding. Canadian Journal of Urology. PubMed.
12. Elterman et al. (2020). Transfusion rates after 800 Aquablation procedures using various haemostasis methods. BJU International. DOI.
13. Nguyen et al. (2020). Waterjet ablation therapy for endoscopic resection of prostate tissue trial (WATER) vs WATER II: Comparing Aquablation therapy for benign prostatic hyperplasia in 30–80 and 80–150 mL prostates. BJU International. DOI.
14. Plante et al. (2019). Symptom relief and anejaculation after aquablation or transurethral resection of the prostate: Subgroup analysis from a blinded randomized trial. BJU International. DOI.