Cameron Lesions: Often Overlooked
While large hiatal hernias are well known to cause heartburn, vomiting and regurgitation, their role in causing iron deficiency anemia is easily overlooked.
One 68-year-old male went years receiving treatment for his anemia of “unknown origin” with regular iron infusions and blood transfusions. It wasn’t untill he sought care for debilitating symptoms of acid reflux and vomiting from Seth A. Gross, MD, clinical chief of the Division of Gastroenterology and Hepatology, that the cause of both his gastrointestinal issues and anemia was revealed.
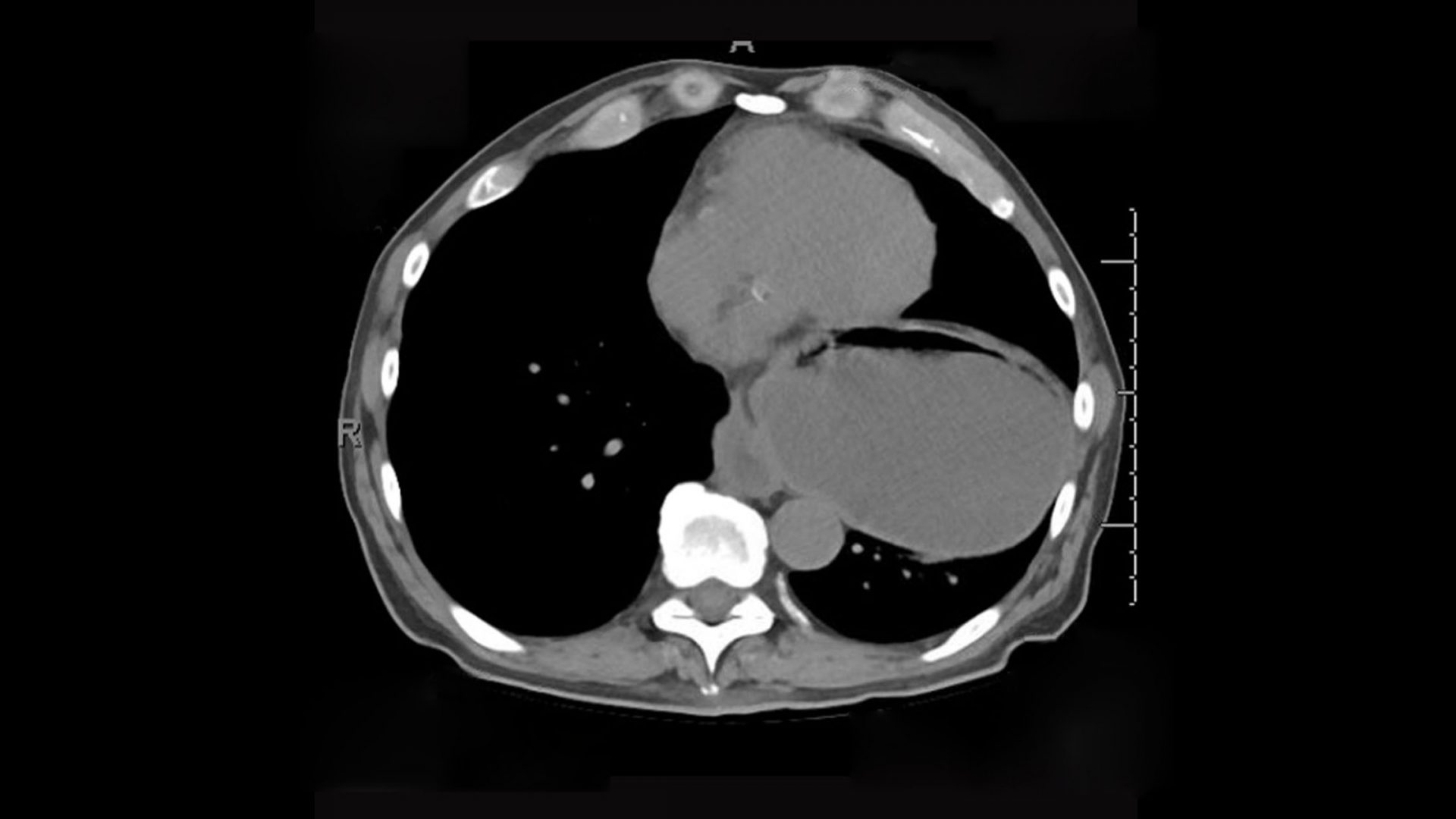
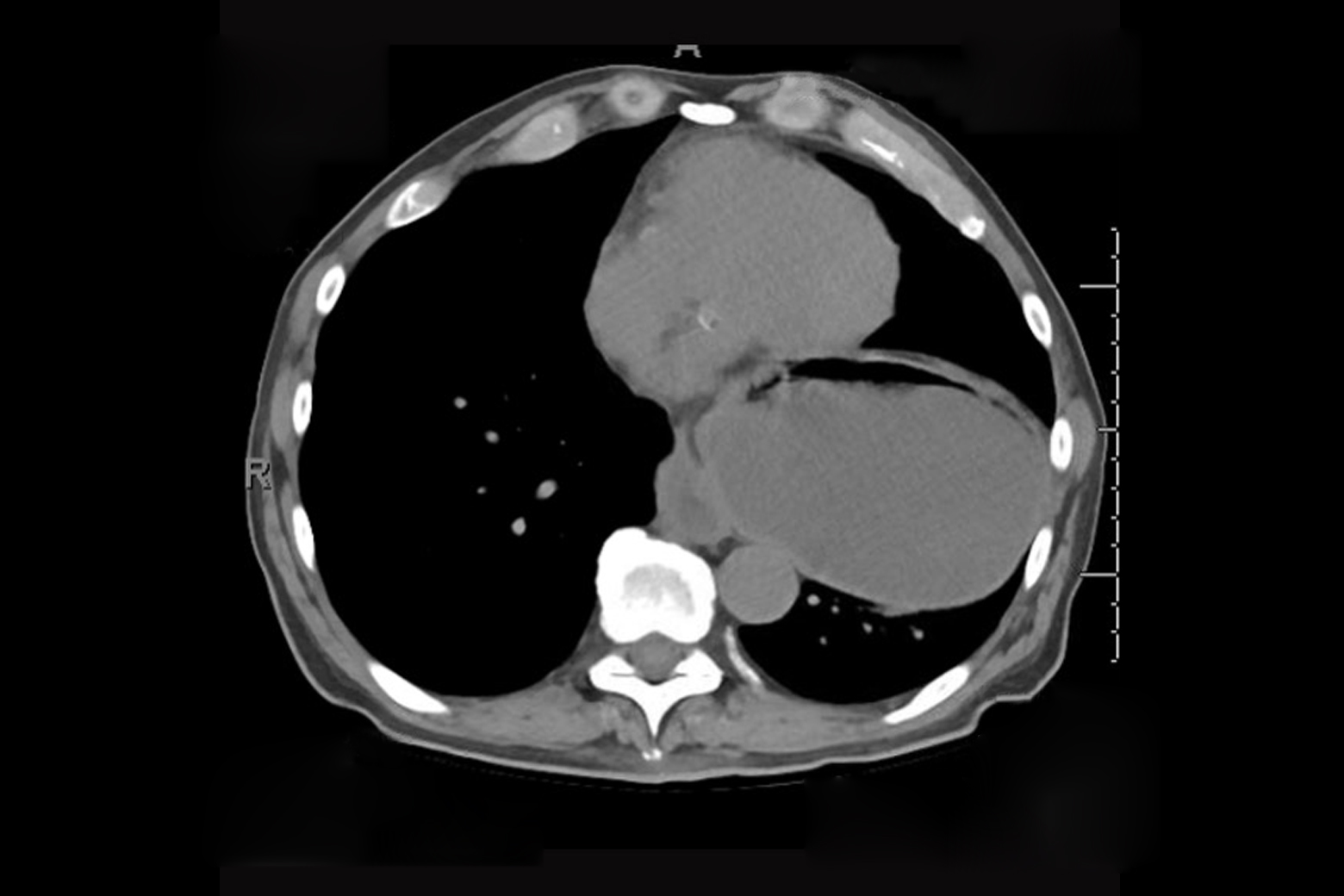
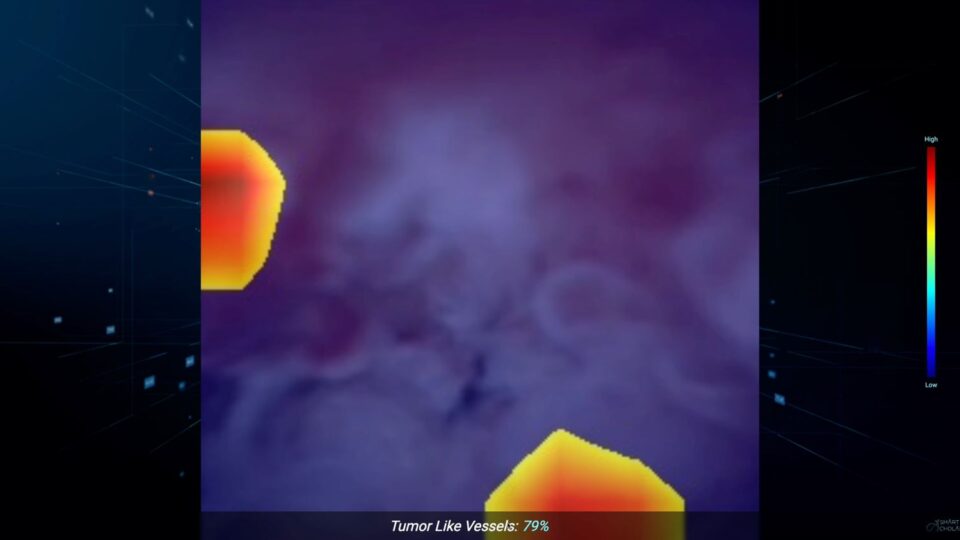
After detecting a large hiatal hernia, Dr. Gross made the connection that not only was the hernia affecting the patient’s ability to keep food down, but Cameron lesions, or gastric ulcers that result from the recurrent sliding of the stomach across the opening of the diaphragm, were causing chronic blood loss.
“When I did the endoscopy, I saw this irritation or break in the lining where part of the hernia was coming through the diaphragm, indicative of a Cameron erosion,” Dr. Gross explains.
“When I did the endoscopy, I saw this irritation or break in the lining where part of the hernia was coming through the diaphragm, indicative of a Cameron erosion.”
Seth A. Gross, MD
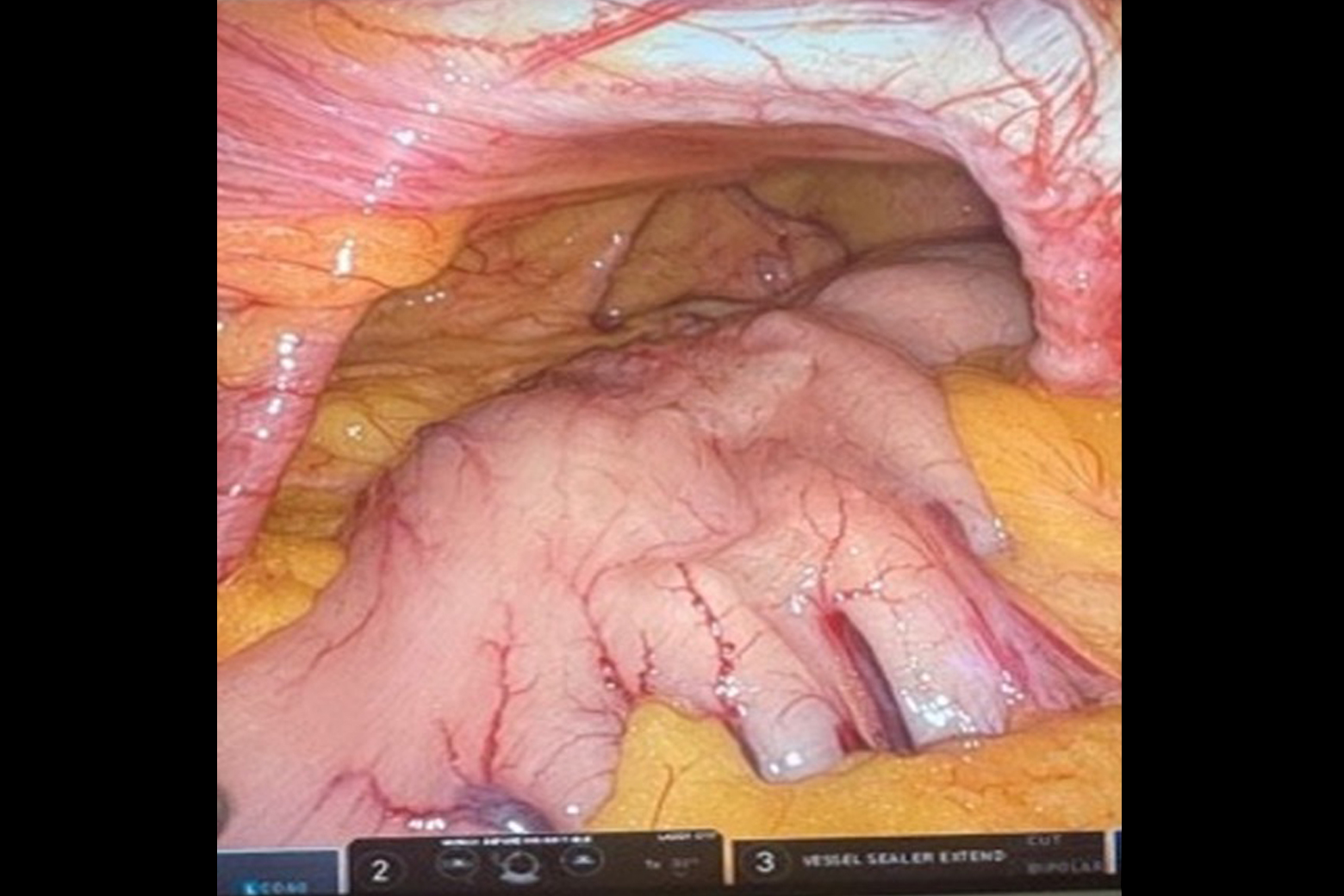
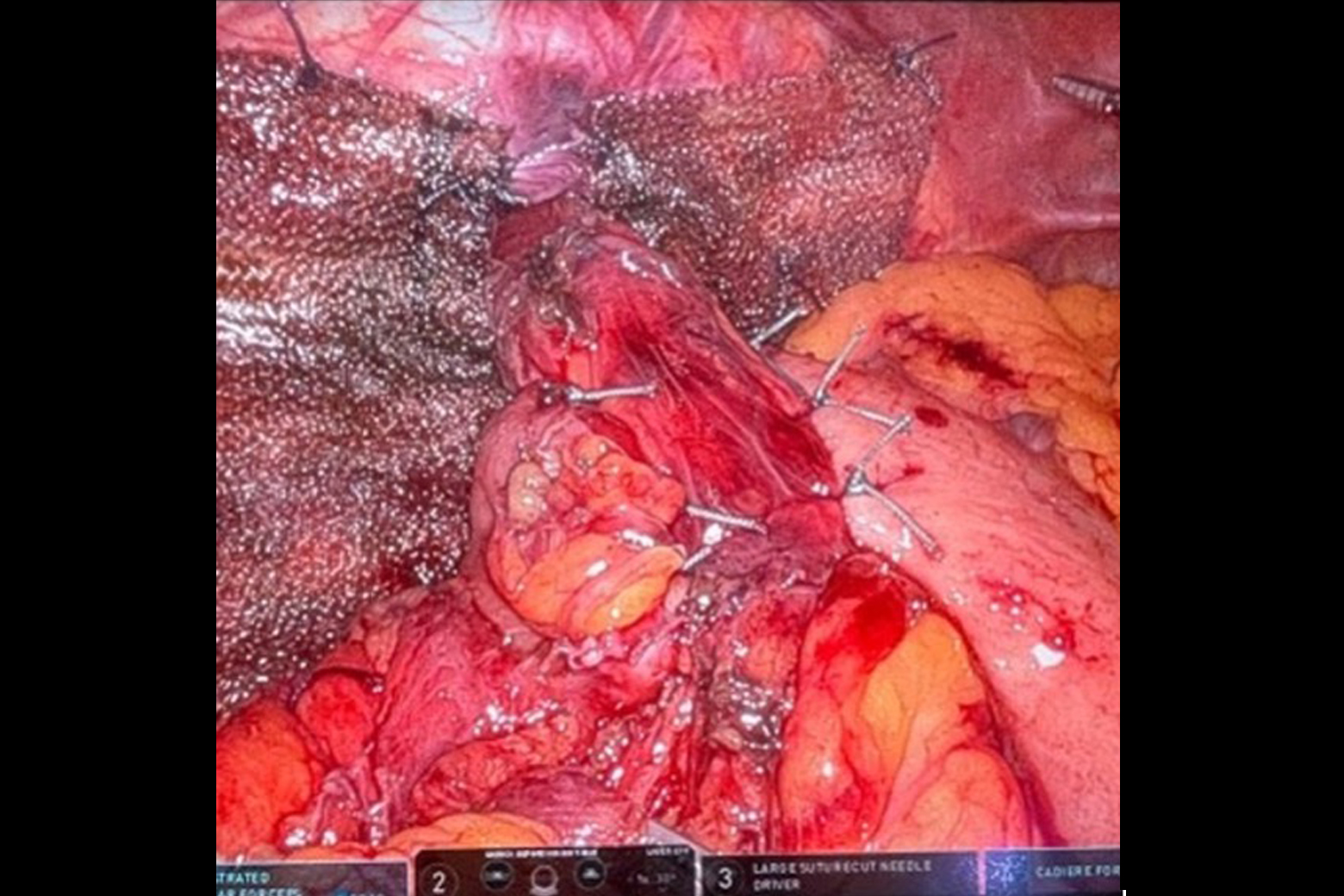
Tanuja Damani, MD, surgical director of the Center for Esophageal Health, then performed a minimally invasive robotic paraesophageal hernia repair, which resolved both the patient’s anemia and gastrointestinal issues.
“Every patient that we see is evaluated in a multidisciplinary fashion,” Dr. Damani says. “Having Dr. Gross as the advanced endoscopy specialist who studied the anemia further, having the patient’s hematologist within our system, and our expertise in diagnosing and managing paraesophageal hernias really helped steer the care for this patient in the right direction.”