At NYU Langone Health’s Center for Esophageal Health, experts provide highly specialized care for patients with complex conditions of the esophagus and persistent, challenging symptoms that require advanced diagnosis and treatment. The center is co-led by Tanuja Damani, MD, who serves as surgical director, and Abraham R. Khan, MD, the medical director.
In collaboration with Luis F. Angel, MD, medical director of lung transplantation, and Darya Rudym, MD, an assistant professor of medicine, the team has pioneered a multidisciplinary approach to perform timely pre-transplant diagnostic testing for gastroesophageal reflux disease (GERD) and, if needed, endoscopic or surgical intervention to resolve the reflux. They also perform post-transplant diagnostic testing and treatment as needed.
Here, Dr. Damani and Dr. Khan discuss their unique approach to testing and provide a real case example to illustrate the process.
Pulmonary Manifestations of Reflux
Physician Focus: What is the role of chronic pathologic GERD in lung transplant?
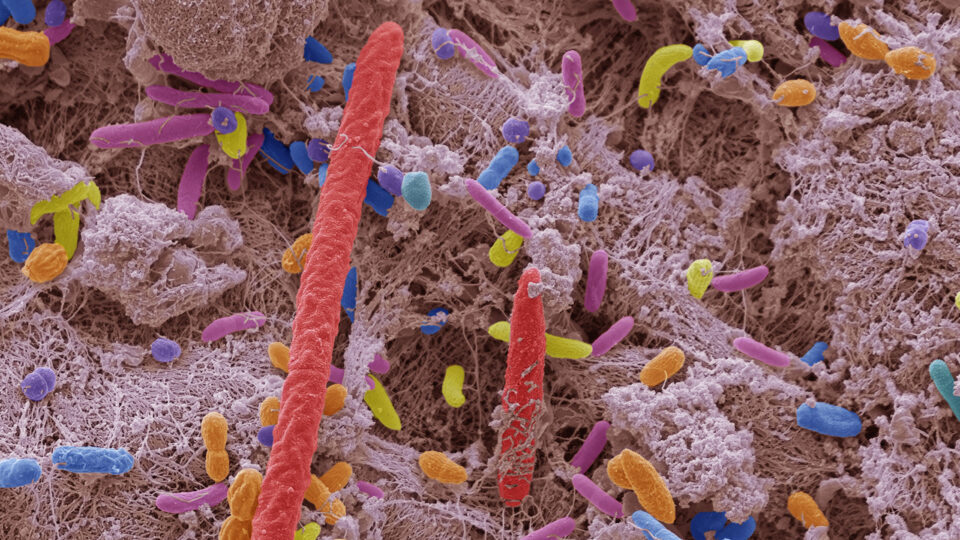
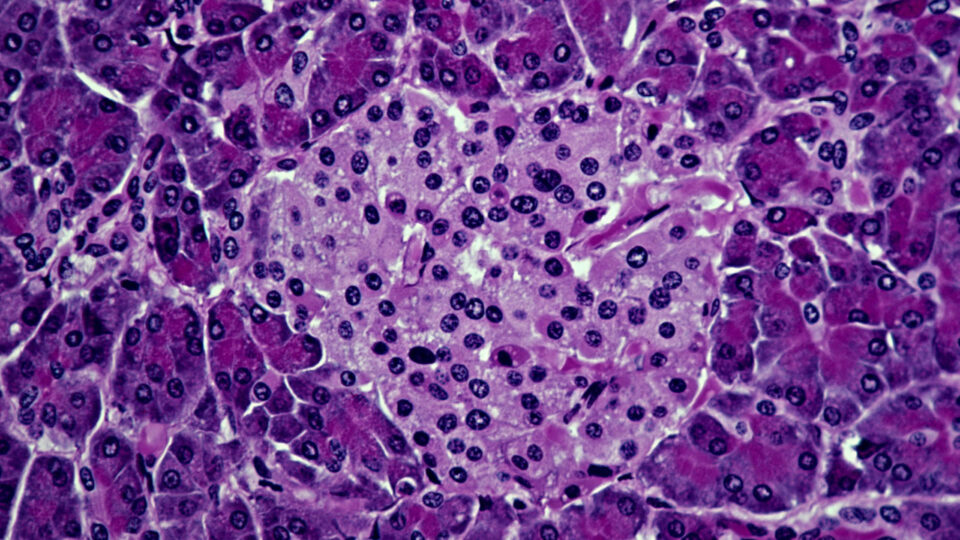
Dr. Khan: Chronic gastroesophageal reflux and the potentially associated microaspiration can exacerbate many chronic pulmonary conditions including asthma, interstitial pulmonary fibrosis, and bronchiectasis. Current guidelines suggest lifestyle modifications and acid-suppressive therapy as first-line treatment options, but these interventions are often insufficient for complex patients, such as those undergoing lung transplant.
Additionally, the use of acid-suppressive therapy alters the pH of gastric contents without fully addressing the consequences of aspiration into the airway, which can be concerning for some transplant recipients, as we want to prevent reflux-driven damage to the lung allograft and reduce the risk of rejection post-transplant.
“In lung transplant recipients, anti-reflux surgery has been shown to reduce the risk of chronic allograft dysfunction, and thus it is important that low-risk minimally invasive surgery be considered for these patients.”
Tanuja Damani, MD
Dr. Damani: Adding to what Dr. Khan said, severe reflux and regurgitation that cannot be medically managed often jeopardize the longevity of the new lungs due to reflux-induced microaspiration and resulting inflammation. In lung transplant recipients, anti-reflux surgery has been shown to reduce the risk of chronic allograft dysfunction, and thus it is important that low-risk minimally invasive surgery be considered for these patients.
Streamlined Testing and Treatment
Physician Focus: What is unique about your approach to pre- and post-transplant diagnostic testing for reflux?
Dr. Khan: Our team is actively working to identify all patients with severe GERD in the pre-transplant setting. One unique aspect of our approach is that we incorporate state-of-the-art diagnostic tools into the workup. These awake diagnostic tests can give insights into why the patient has gastroesophageal reflux, and then allow us to understand if that reflux is indeed at risk of aspirating into the airway.
Based on these findings and a detailed, personalized interpretation of testing results, we can determine which patients are at increased risk of reflux-driven damage to the new lungs and who may benefit from treatment, whether that be medical or surgical and conducted pre- or post-transplant.
“Our team is actively working to identify all patients with severe GERD in the pre-transplant setting. One unique aspect of our approach is that we incorporate state-of-the-art diagnostic tools into the workup.”
Abraham R. Khan, MD
Dr. Damani: From a surgical perspective, our goal is to optimize the transition from diagnosis to surgery, and to determine which types of patients with reflux may benefit from intervention. We prefer to perform robotic anti-reflux surgery within 30 to 60 days following lung transplant to minimize any damage from reflux to the new lungs.
Our approach is unique in that we truly function as a multidisciplinary team. We hold biweekly lung transplant meetings, which include pulmonologists, esophagologists, and surgeons, where we discuss patients that were previously identified. This allows us to expedite the GERD workup, both pre- and post-transplant.
We have also developed secure chat groups on Epic and other platforms that allow for more seamless flows of information and expedited scheduling between the specialist teams for these patients.
An Early Glimpse of Success
Physician Focus: Dr. Damani, do you have any recent examples of success using this approach?
Dr. Damani: Yes. We had a male in his 70s who underwent bilateral lung transplant for interstitial pulmonary fibrosis. He had severe reflux and regurgitation that could not be medically controlled. Shortly after his transplant, he underwent an extensive GERD workup by our esophageal team and we elected to perform a robotic fundoplication. Overall, he did fantastic despite being on immunosuppression and was discharged two days after surgery on no pain medications. He has a great quality of life now, is off all his reflux meds, and is residing back home in Colombia.
A Vision for the Future
Physician Focus: Since seeing early success using this approach, what are your future goals?
Dr. Khan: Utilizing our current pre-lung transplant protocol, we hope to add to the sparse body of literature that pertains to the treatment of GERD in lung transplant patients. Our future aim is to identify the most appropriate medical and surgical therapies for GERD and esophageal motility disorders, both before and after transplant, that lead to successful long-term outcomes.
“Our testing approach shows great promise to improve long-term outcomes for lung transplant patients. As we collect and analyze more data, we hope to disseminate these findings.”
Dr. Damani
Dr. Damani: Our testing approach shows great promise to improve long-term outcomes for lung transplant patients. As we collect and analyze more data, we hope to disseminate these findings through publications in peer-reviewed journals and conference presentations—this would greatly benefit the broader scientific and medical communities.