Laura Balcer, MD, is a professor of neurology, ophthalmology, and population health, and vice chair of the Department of Neurology. An internationally renowned researcher and author of more than 350 publications, Dr. Balcer is editor-in-chief of the Journal of Neuro-Ophthalmology. Here, Dr. Balcer discusses her perspectives on advancements in the field and where neuro-ophthalmology is heading.
Physician Focus: You’ve been appointed editor-in-chief of the Journal of Neuro-Ophthalmology. From the research the journal is publishing and the work you and your colleagues are doing at NYU Langone Health, what is on the forefront for the field?
Dr. Balcer: There is very exciting work happening in Alzheimer’s and other neurodegenerative diseases. Expanded applications of optical coherence tomography (OCT) and other vision-based diagnostic tools are providing new insights into the effects of these disorders on the eye and visual pathway. Some of the types of tests we are investigating, such as rapid picture-naming, or mobile universal lexicon evaluation system (MULES) and rapid number-naming, or staggered uneven number (SUN), have been around for over 80 years, and can potentially help to predict disease progression.
Here at NYU Langone, we are leading collaborative sub-studies of clinical trials that will use OCT, as well as MULES and SUN, to identify markers for Alzheimer’s and Parkinson’s disease. Additionally, we have expanded the applications of OCT and of low-contrast letter acuity (eye charts with gray letters on a white background) to the evaluation of other conditions, such as multiple sclerosis (MS) and suspected chronic traumatic encephalopathy (CTE) or concussion in athletes.
There is much research being done on COVID-19 and its impact on the central nervous system. Researchers have been evaluating the accelerated use of tele-neuro-ophthalmology over the last two years and how it will impact future neurology and ophthalmology practice.
OCT as a Diagnostic Tool in MS
Physician Focus: You have made significant breakthroughs in the study and early treatment of MS. How is OCT being used as a tool for diagnosing this neurological disorder?
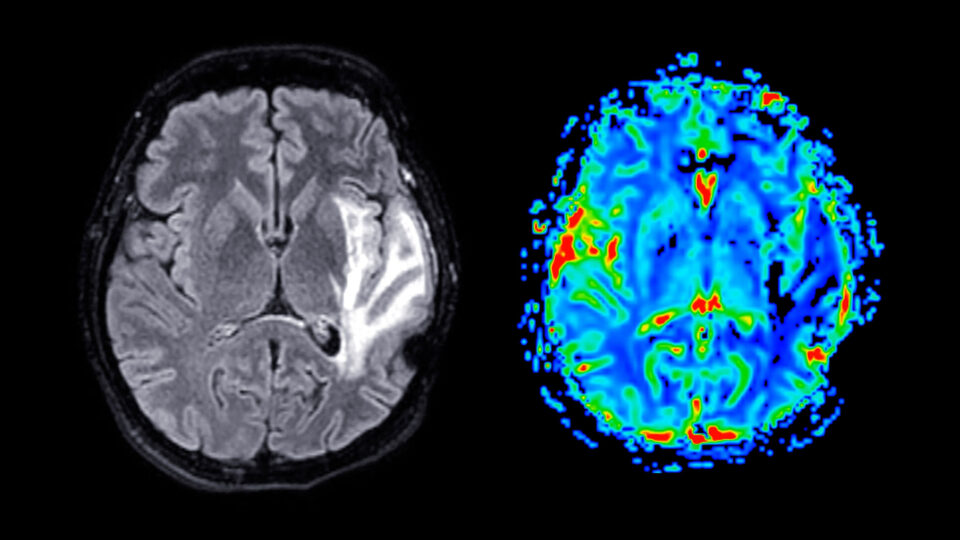
Dr. Balcer: We think physical changes in the visual system may be structural markers for neurological disease. Because OCT is non-invasive and relatively easy to use, we can now image structures in the eye that reflect what is going on in the rest of the visual system and potentially in the brain overall. OCT captures images and quantitative thicknesses in the optic nerve head, the retinal nerve fiber layer (axons), and cellular layers of the macula.
In MS, the higher resolution of OCT scans may be better able to detect both asymptomatic and symptomatic optic nerve lesions. The optic nerve, despite many patients having inflammation of this structure as a first clinical event in MS, is not yet included as a lesion site in the diagnostic criteria for MS. We are working to change that, with worldwide collaborations and investigations with ocular imaging teams right here at NYU Langone that pioneered OCT.
In 2018, we conducted a study that established a threshold for inter-eye differences in degrees of retinal nerve fiber layer and macular thinning that signals a patient has had acute optic neuritis. These inter-eye difference thresholds measured by OCT will be complementary to magnetic resonance imaging in identifying optic nerve lesions.
This investigation led to an international, multisite study of 1,530 patients with MS that confirmed the inter-eye difference thresholds for the identification of an optic nerve lesion within a larger and more diverse study cohort.
As part of our ongoing MS research, we recently published a study using the world’s largest MS database which demonstrates that early treatment with MS therapies is associated with lower risk of conversion to MS and improved neurological/visual function in patients with optic neuritis.
Vision Testing and Cognitive Decline
Physician Focus: In another emerging research area, what can OCT tell us about CTE and concussion? Are there other new diagnostic tools?
Dr. Balcer: In individuals with a history of repetitive head traumas, such as contact sport athletes, the goal is to determine whether the visual pathway can serve as a potential living biomarker for CTE or cognitive decline among those who have a history of contact sports exposure. NYU Langone is one of four study sites for an NIH-funded investigation led by researchers at Boston University to develop criteria for traumatic encephalopathy syndrome—a potential phenotype in living persons at risk for CTE.
In a partnership with NYU Langone’s Concussion Center, we are involved in ongoing research on the use of the MULES and SUN tests. These tests, under investigation as research paper/pencil or as part of a research tablet application, were developed at NYU Langone and have shown worse time scores among athletes with concussion on the sideline in the setting of more chronic concussion, and in patients with MS, mild cognitive impairment due to Alzheimer’s, Parkinson’s, and long-haul symptoms of COVID-19. The MULES, SUN and other rapid automatized naming tasks likely require different brain pathways and networks for visual processing, visual memory, language, and eye movements.
Broadening the Field’s Impact
Physician Focus: Any closing thoughts as you enter this next chapter in your career?
Dr. Balcer: We are excited to be neuro-ophthalmologists, since we have learned that vision is a potential avenue to measuring disease and outcomes in areas with both an established repertoire of clinical trials and treatment, and for those fields that are just starting to have effective therapies.
The teams at NYU Langone are incredibly collaborative and supportive. We are making tremendous progress in the evaluation and treatment of our patients through the capacity to share knowledge and advancements within and beyond our field. We are grateful to our very knowledgeable and innovative colleagues in neuroradiology, ophthalmology, neuropathology and other specialties. We are also delighted to continue to mentor through our Patient-Oriented Research Curriculum for residents, and to teach trainees about the fundamentals of clinical research. And of course, the impact of the pandemic on neurological training has been an important opportunity to teach our colleagues in neurology how to pivot under circumstances of adversity.