An automated system that flags patients who could most benefit from mineralocorticoid receptor antagonists (MRAs), lifesaving drugs for heart failure, more than doubled new prescriptions, according to a pilot program tested by researchers at NYU Langone Health.
The study, recently presented at the annual conference of the American College of Cardiology and simultaneously published in the Journal of the American College of Cardiology, is the first to directly compare the effectiveness of alert message types that address heart failure.
“Our findings suggest that tailored electronic notifications can boost the prescription of lifesaving drugs.”
Amrita Mukhopadhyay, MD
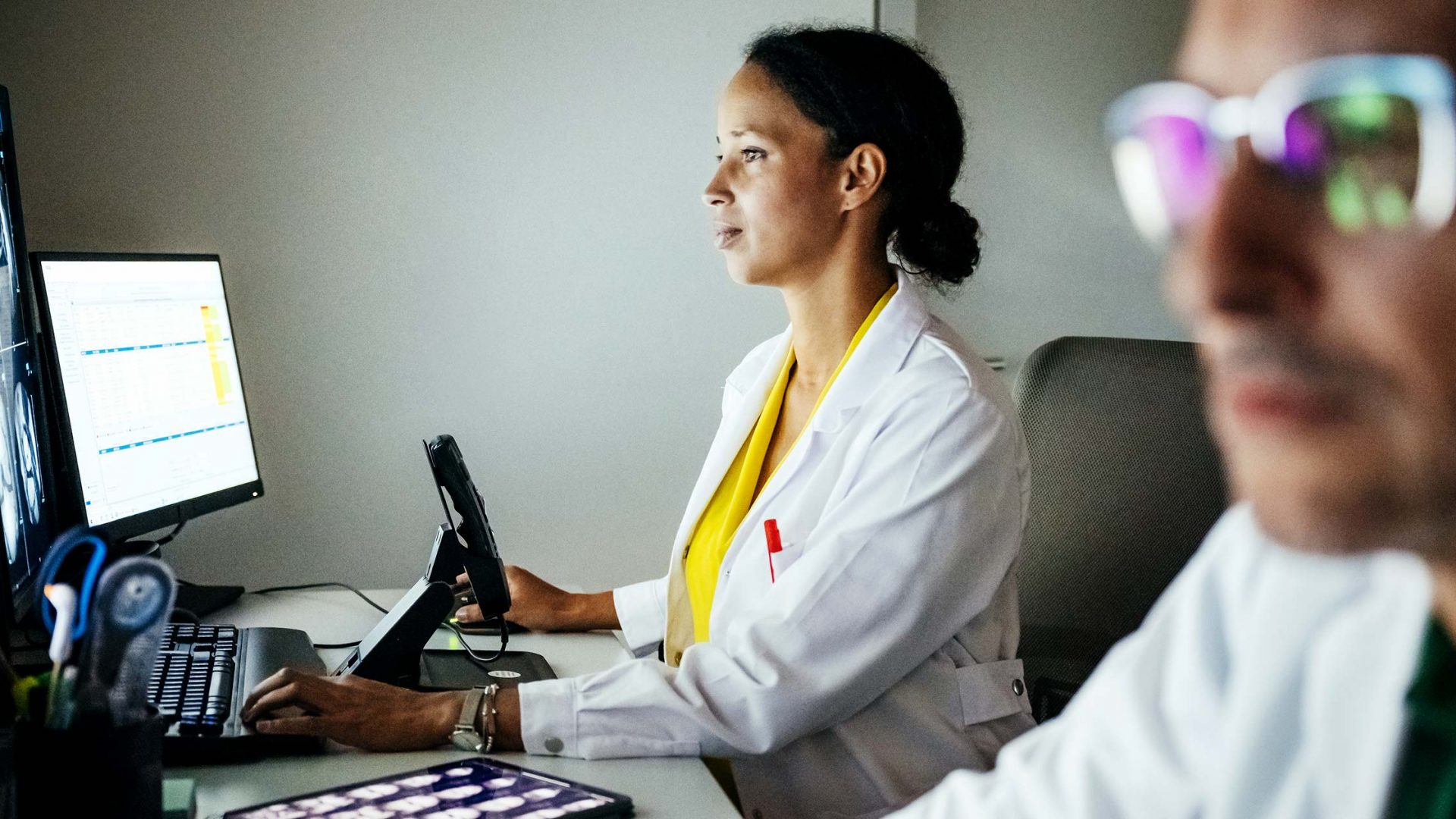
“Our findings suggest that tailored electronic notifications can boost the prescription of lifesaving drugs,” says study lead author and cardiologist Amrita Mukhopadhyay, MD, a clinical instructor in the Department of Medicine.
“By compiling key information in one place, the system may help providers spend less time searching through medical records during a visit and more time speaking with their patients.”
Testing the Potential of Automated Alerts
While MRAs can greatly increase heart failure survival rates, past studies have shown that almost two-thirds of eligible patients are not prescribed these drugs, says Dr. Mukhopadhyay.
Part of the challenge in prescribing MRAs is that the medical information needed to determine a patient’s eligibility is scattered throughout their electronic health record. As a result, experts have been exploring the use of digital messaging tools that automatically analyze standard clinical guidelines and relevant medical data to make treatment decisions easier.
“Well-designed electronic tools can be a rapid, low-cost, and impactful way to improve care.”
In the new study, the researchers designed a pilot program to find the most effective type of digital alert, testing two automated technologies over six months.
For one of the technologies, alerts appeared on the top corner of patient healthcare charts, which are routinely reviewed during visits. They included data that may inform decisions about MRA therapy, such as blood pressure, estimated glomerular filtration rate, and potassium levels in the blood.
For the other technology tested, cardiologists received a monthly message within the healthcare system’s internal messaging platform that included a list of those eligible for MRAs. Through this “email,” healthcare providers could open medical charts and read information relevant for prescribing MRAs.
Between April and October 2022, the research team tested the notification systems at more than 60 cardiology outpatient clinics.
Strong Support for Digital Messaging
The results showed that cardiologists who received a banner-like alert on their computer screen prescribed MRA therapy for about 30 percent of their patients over the course of the trial. Those who were instead sent monthly email-like messages prescribed MRA therapy roughly 16 percent of the time. By contrast, those who received neither type of message prescribed the therapy for 12 percent of their patients.
“Well-designed electronic tools can be a rapid, low-cost, and impactful way to improve care,” adds Dr. Mukhopadhyay.
While the results are highly promising, the researchers caution that this technology was only tested in cardiology practices within a large urban healthcare system. The team plans to explore the effectiveness of these tools in other settings in the future.