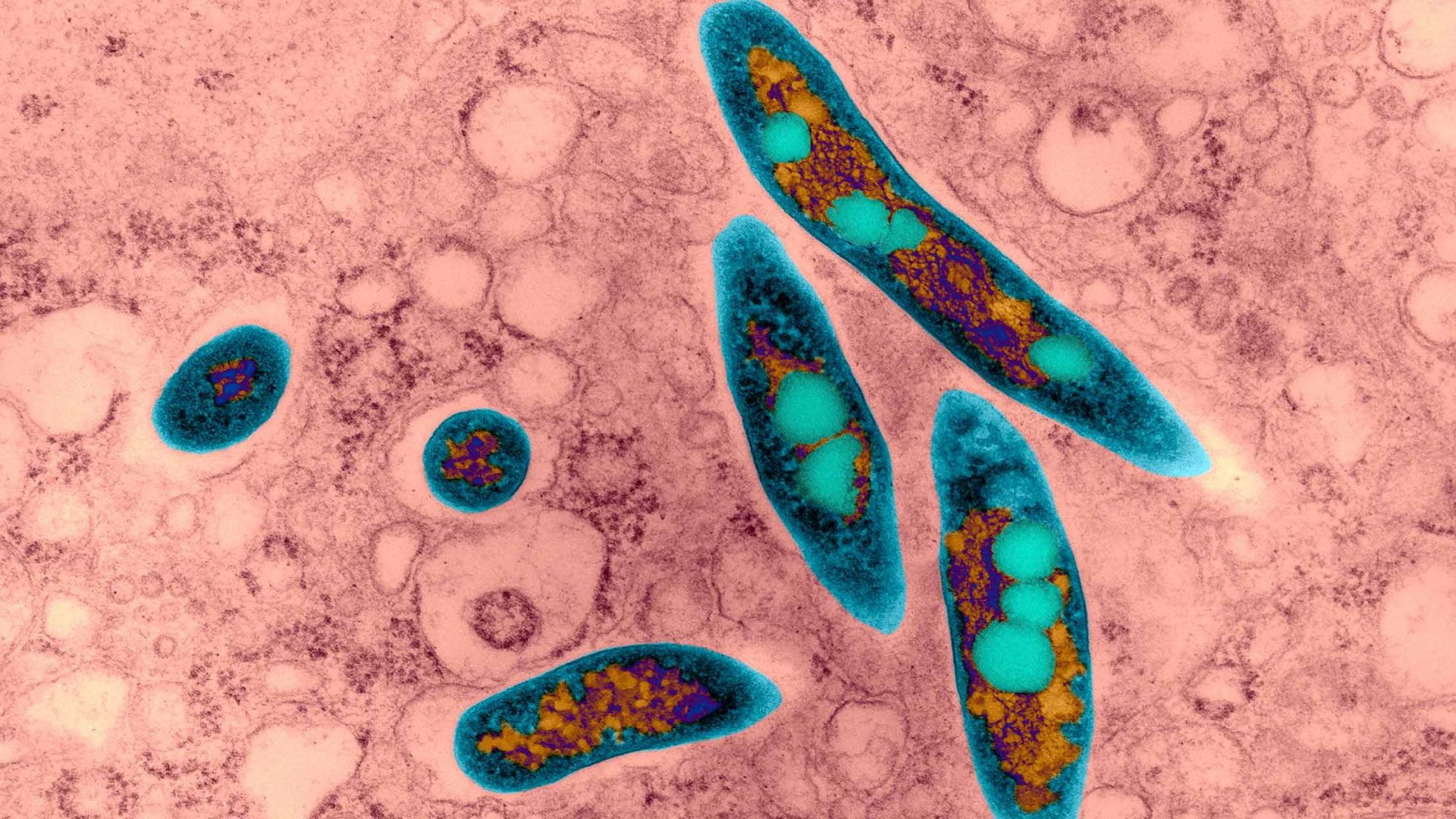
Bronchiectasis is characterized by chronic cough and marked by thickened, dilated airways on CT scan. Airway dilation can cause cilia impairment, failure of mucus clearance, increased risk of infection, and airway obstruction, leading to impaired lung function. The lungs of people with bronchiectasis are often colonized by harmful fungi and bacteria, including nontuberculous mycobacteria (NTM).
“Awareness of bronchiectasis and NTM lung disease has increased, as have incidence and prevalence,” says Doreen J. Addrizzo-Harris, MD, co-director of NYU Langone Health’s Bronchiectasis and NTM Multidisciplinary Program, a leading center in the management of bronchiectasis and NTM infection. “While diagnosis is often delayed two to three years or more, with increased use of chest CT scans and advanced microbiology laboratories, diagnosing these patients has improved in recent years.”
Dr. Addrizzo-Harris and the program are actively involved in research initiatives to better understand these conditions. Despite medical therapy being effective in up to 75 percent of NTM cases, she says, some NTM infections are difficult to treat and require innovative therapies.
“The goal is to treat the majority of patients based on the newest guidelines, and for those with complex cases to develop personalized treatments based on clinical outcomes, microbiology, and biomarkers.”
Doreen J. Addrizzo-Harris, MD
“Every patient with bronchiectasis and NTM infection is different,” Dr. Addrizzo-Harris says. “The goal is to treat the majority of patients based on the newest guidelines, and for those with complex cases to develop personalized treatments based on clinical outcomes, microbiology, and biomarkers.”
Better Identifying Subtypes of Bronchiectasis
There are many causes of bronchiectasis, says Dr. Addrizzo-Harris. “It could be congenital, such as cystic fibrosis (CF) or immunoglobulin deficiencies. Or it could be caused by prior infection, chronic aspiration, ciliary abnormalities, alpha-1 antitrypsin disease, rheumatologic disease—the list goes on.”
New biomarker research is applying emerging phenotyping and endotyping techniques to identify the patient populations who would most benefit from specific treatments, with the goal of better targeting new treatments directed at infection, inflammation, and other aspects of the disease cycle.
Dr. Addrizzo-Harris works closely with Leopoldo N. Segal, MD, director of the Translational Lung Biology Laboratory, in analyzing the lung microbiome to determine patterns that may give clues to better ways of treating patients with NTM infection.
“Do we need to treat the bacteria, or is there something we need to treat that is in the white blood cell and part of the inflammatory cascade? That’s the thought right now,” Dr. Addrizzo-Harris says.
Improving NTM Treatment
It is critical to get frequent sputum samples in patients diagnosed with bronchiectasis to evaluate for harmful organisms, Dr. Addrizzo-Harris notes.
“Which starts first—the NTM or the bronchiectasis? CT scan can reveal infection, but if you don’t get sputum, you won’t find these and some of the fungal infections associated with bronchiectasis such as aspergillosis.”
Antimicrobial sensitivity testing or erm gene analysis may be necessary, explains Dr. Addrizzo-Harris, as NTM species and subspecies have varying susceptibility to existing antibiotics, including macrolides.
“Before, non-CF bronchiectasis and NTM infection were considered rare and had very little support. Now, with new drugs targeted at these areas of pathophysiology that have been identified, we hope to move faster in developing effective treatments.”
Several new drugs hold promise for treating NTM infections, with antimicrobials apramycin, epetraborole, and omadacycline currently in trial. NYU Langone researchers participated in a study of inhaled liposomal amikacin for treatment of Mycobacterial avium complex that demonstrated 30 percent increase in sputum conversions and longer durability in approximately 50 percent of patients.
Bacteriophages have demonstrated favorable clinical outcomes in a preliminary trial in patients lacking other options. NYU Langone researchers have published a pilot trial using robotic surgery as a viable option for patients requiring lung resection.
“Before, non-CF bronchiectasis and NTM infection were considered rare and had very little support,” Dr. Addrizzo-Harris says. “Now, with new drugs targeted at these areas of pathophysiology that have been identified, we hope to move faster in developing effective treatments.”
Clinical and Translational Research
Dr. Addrizzo-Harris is joined by David L. Kamelhar, MD, Ashwin Basavaraj, MD, and Stephanie Lau, MD, in conducting a prospective evaluation of patients with NTM infection and collecting clinical and survey data to facilitate study of the disease process. Dr. Segal is developing a biorepository of airway samples collected during antimycobacterial treatment.
NYU Langone is the largest contributor of patient data to the COPD Foundation’s Bronchiectasis and NTM Research Registry.