Jun Tashiro, MD, MPH, a board-certified pediatric surgeon who specializes in bariatric surgery, discusses the role of surgery in adolescents with obesity—a highly prevalent condition that has more than tripled in the past three decades. In the wake of the pandemic, anxiety and stress have also hindered efforts to address obesity.
Working with a multidisciplinary team, Dr. Tashiro gives teens the tools they need to achieve and maintain a healthy weight through the Adolescent Healthy Weight Program, where he serves as surgical director.
Impact of the Pandemic on Obesity Trends
Physician Focus: How has the COVID-19 pandemic affected weight management and care of adolescents with obesity?
Dr. Tashiro: According to a recent study from the CDC, the rate of increase in children and teens’ body mass index (BMI) approximately doubled in 2020—obesity was an epidemic already, but the pandemic has made it much worse.
With schools closed and gym classes cancelled, kids lost their normal routine. Although this was necessary for public health, we don’t talk enough about the importance of a structured school day for children—their entire world involves interacting with friends, and if you take that away, and only put them in front of a screen, it’s not the same.
Weight Management Care for Youth
Physician Focus: The Adolescent Healthy Weight Program at NYU Langone provides a care experience with unique benefits to young patients. Can you tell us more about it?
Dr. Tashiro: There are many weight loss programs available to patients, but most surgical procedures are not performed by pediatric surgeons subspecialized in bariatric surgery.
At Hassenfeld Children’s Hospital at NYU Langone, all of our pediatric patients receive specialized care from initial consultation through to treatment and follow-up. We employ a multidisciplinary care team, including pediatric obesity medical specialists, nutritionists, psychologists, social workers, and subspecialized pediatric surgeons.
We ensure that our patients are treated as teenagers—15-year-olds should not be talked to and treated the same way as adults. A children’s hospital can offer a unique care experience for teens. Our program is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program as a comprehensive center providing high-quality, patient-centered care.
The Proven Benefits of Surgery
Physician Focus: There is accumulating evidence suggesting that bariatric surgery is safe and beneficial for teens with obesity. Have you published any recent research on this topic?
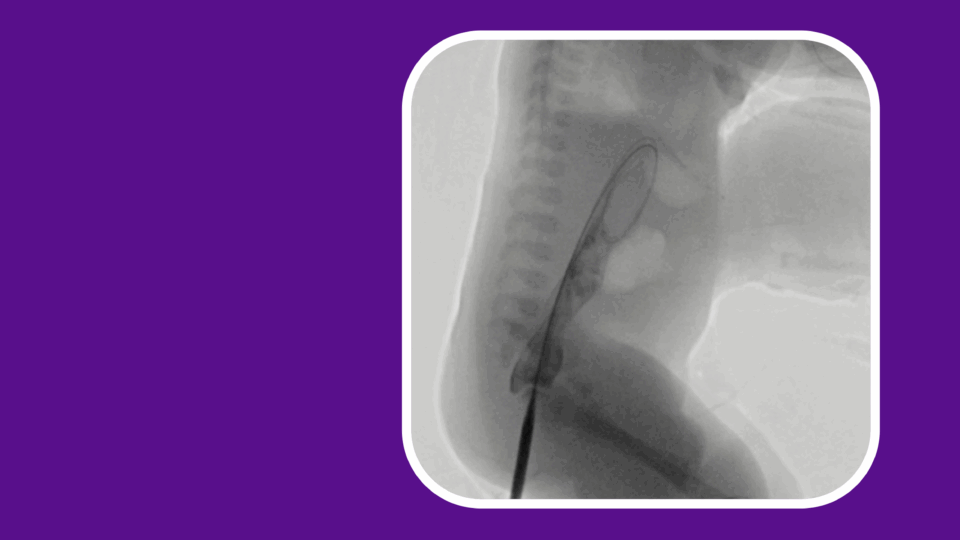
Dr. Tashiro: We recently published the results of a retrospective analysis evaluating the impact of parental history of bariatric surgery, as well as age at time of operation, on adolescents who underwent laparoscopic sleeve gastrectomy.
Interestingly, when all patients were compared by age at operation, either over the age of 16 or under, there were few differences in outcomes. Our results showed that patient age should not be a barrier to weight loss surgery, especially among patients with a parental history of obesity. By intervening at a younger age, the long-term metabolic effects of obesity may be reduced.
Giving Surgery Careful Thought
Physician Focus: What are your considerations when counseling patients about potential weight loss surgery?
Dr. Tashiro: Achieving a healthy weight can be challenging, especially for young people who have experienced significant weight gain that is affecting their physical and mental health.
All teens in our program start with medical weight loss interventions. If those efforts prove unsuccessful, we may recommend surgery. This process starts with an evaluation by a psychologist, who determines if the teen is fit for the procedure. We want to ensure the teen fully understands how it will impact their life and is committed to making lifelong changes to maintain weight loss.
We provide gastric sleeve surgery, also known as sleeve gastrectomy, for teens aged 13 to 17 who have a BMI of 40 or higher, or a BMI of 35 or higher and at least one accompanying risk factor, such as diabetes. This procedure reduces the size of the stomach, which helps teens eat less and feel full faster.
Research shows that bariatric surgery helps teenagers lower their BMI and reverse or significantly reduce their risk of type 2 diabetes and heart disease. By reducing the risk of these obesity-related disorders earlier in life, surgical treatment can help prevent illness in teens and lead to better health as adults.
Reaching More Patients
Physician Focus: What are your future plans for program expansion?
Dr. Tashiro: We plan to expand our coverage area for outpatient visits to include more of the New York metropolitan area as it’s easier for patients if they don’t have to travel so far.
We also plan to provide educational materials for all pediatricians in the tri-state area. Many pediatricians don’t know bariatric surgery is a safe and effective option for adolescents with obesity.