Within orthopedics, open fractures have long been viewed as a surgical emergency, irrespective of location, patient characteristics, or the mechanism of injury. After an open distal radius fracture (ODRF), for example, orthopedic surgeons have typically advised urgent irrigation, debridement, and operative fixation.
However, a retrospective analysis led by investigators at NYU Langone Health—the largest of its kind—challenges these practices.
The study, which was named the best hand and wrist paper at the 2023 American Academy of Orthopaedic Surgeons (AAOS) Annual Meeting, finds delaying treatment for an ODRF injury beyond 24 hours does not yield a greater risk of postoperative complications. Age, energy and mechanism of injury, or fracture grade doesn’t alter the outcome in any statistically significant way either.
“The value of this study is that it allows us to start thinking much more scientifically about open fractures. There’s a world of difference between an open femur and an open distal radius.”
Jacques H. Hacquebord, MD
“The value of this study is that it allows us to start thinking much more scientifically about open fractures,” says senior author Jacques H. Hacquebord, MD, co-director of the multidisciplinary Center for Amputation Reconstruction. “There’s a world of difference between an open femur and an open distal radius. We can’t think of them and treat them the same way. What’s good for one might not be good for the other, and vice versa.”
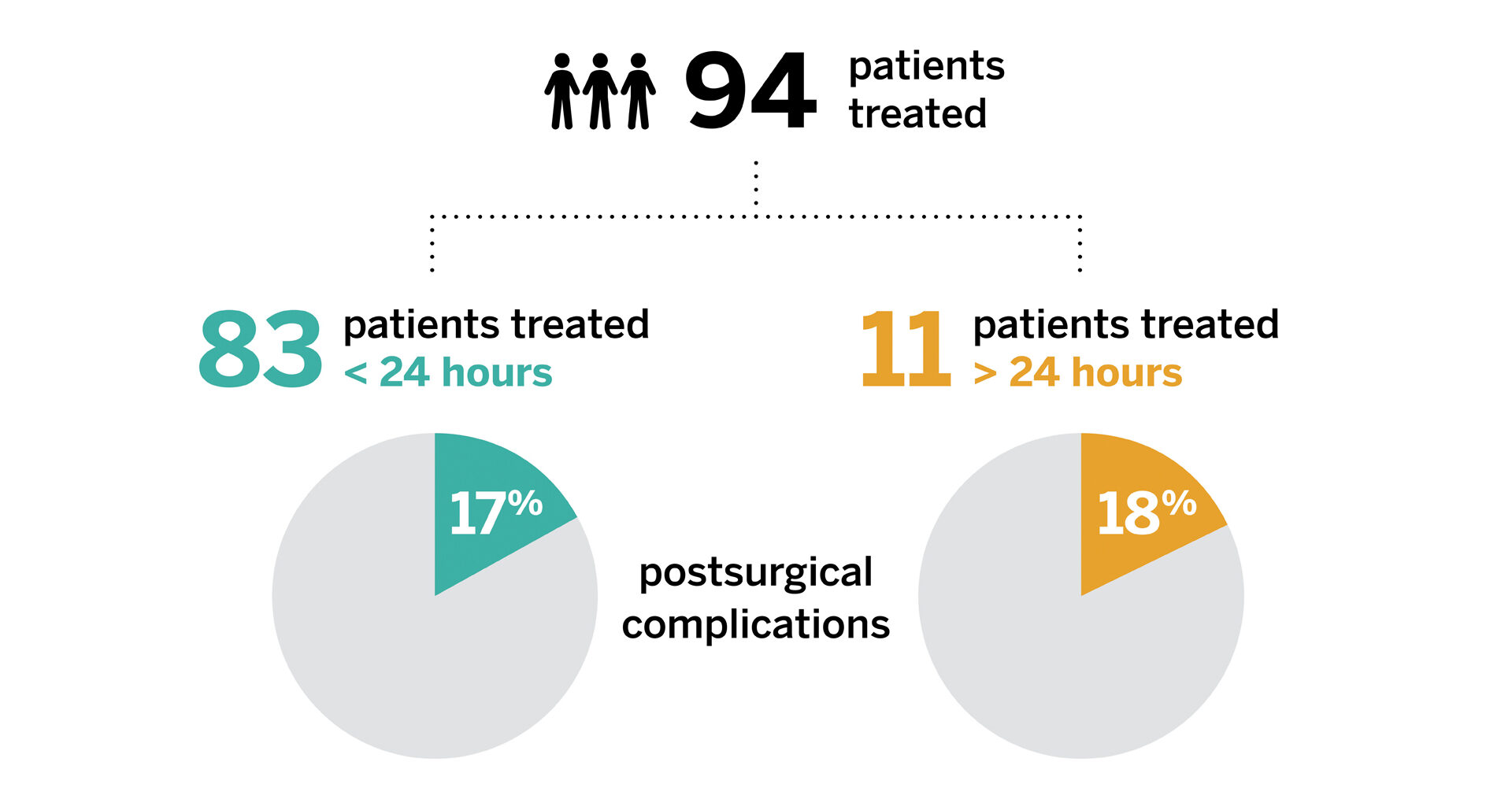
The study, which included 94 patients presenting with an ODRF injury over a six-year period, analyzed the rate of postoperative complications, including surgical site infection, revision irrigation and debridement, delayed soft tissue healing, loss of reduction, and nonunion and malunion. A follow-up national database study by the research team, still underway, has so far pointed to the same conclusions.
Dr. Hacquebord says that similar complication rates regardless of time to treatment have important implications for resource allocation.
“What would be better: for a patient to go urgently to the operating room in the middle of the night with a surgeon who is not a specialist in the area or to be taken to the operating room by a surgeon who is a specialist in the area at a time that’s convenient for the patient?” he says. “I think the latter is much better patient care. That’s what we’ve shown, and people overall have been very excited by our results.”