Novel Hybrid Strategy and Heart Transplant for Infant’s Cardiomyopathy
In September 2022, diagnostic scans taken during the 27th week of an Israeli woman’s pregnancy revealed a severely weakened left ventricle in her developing fetus. The prenatal diagnosis suggested that after birth, the newborn would likely develop severe heart failure and require a heart transplant.
At NYU Langone Health, maternal–fetal medicine and pediatric cardiology specialists confirmed the life-threatening diagnosis of dilated cardiomyopathy via a fetal echocardiogram. At 37 weeks into her pregnancy, the woman gave birth to a baby boy, who was in cardiogenic shock and taken to the Congenital Cardiovascular Care Unit at Hassenfeld Children’s Hospital for specialized care.
“From our perspective, he was very sick,” says Rakesh Singh, MD, medical director of the Pediatric Heart Failure and Transplant Program. “He would need a heart transplant to survive.”
“The donor heart worked perfectly from the moment it started beating.”
T.K. Susheel Kumar, MD
A left ventricular assist device called the Berlin Heart can help a weakened heart move blood through the body, but the device carries an increased risk of bleeding and stroke in infants. To bridge the time until a donor heart would become available, pediatric heart surgeon T.K. Susheel Kumar, MD, proposed a novel alternative that had been used for other congenital heart defects: using the patient’s healthy right ventricle to augment blood flow to the body.
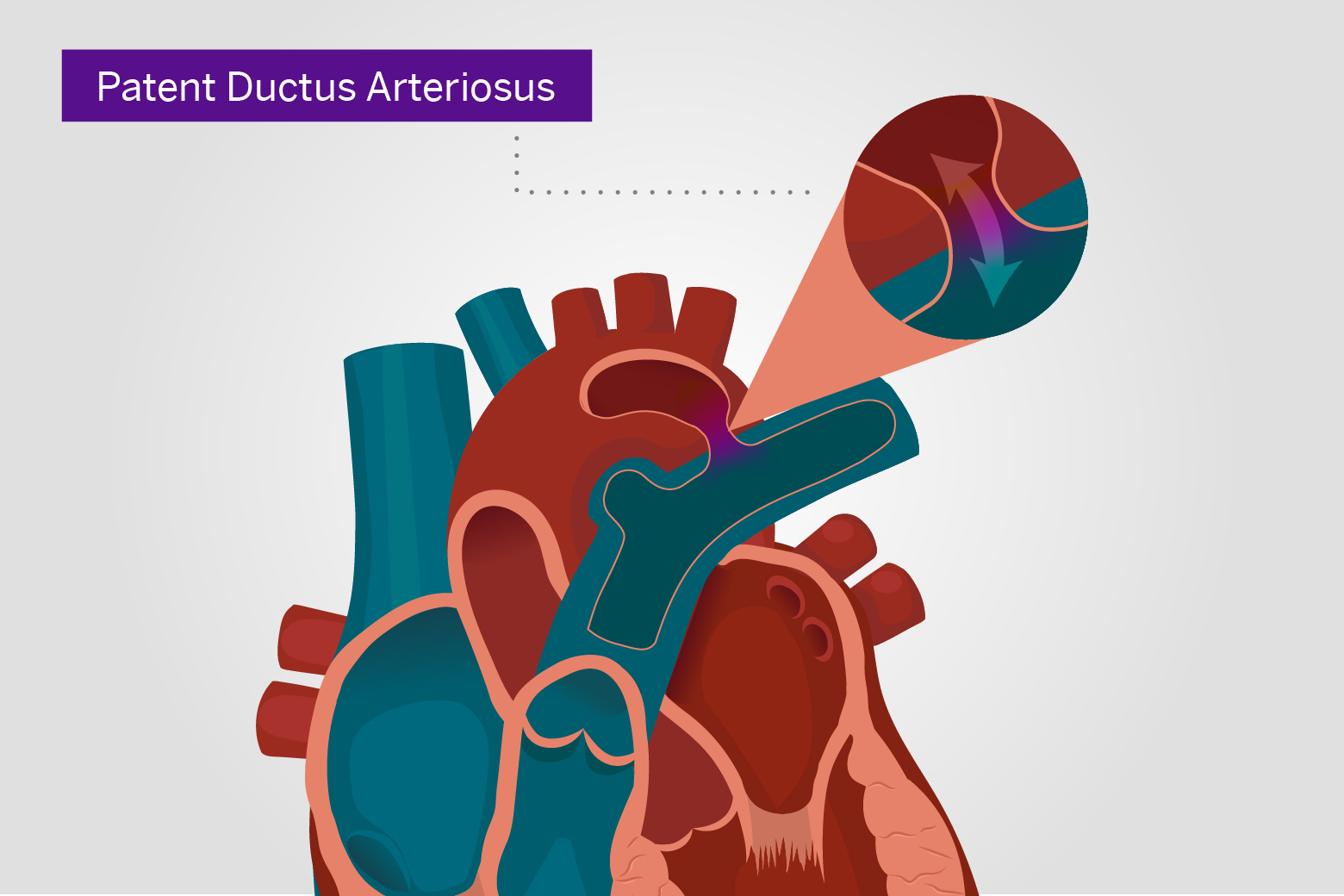
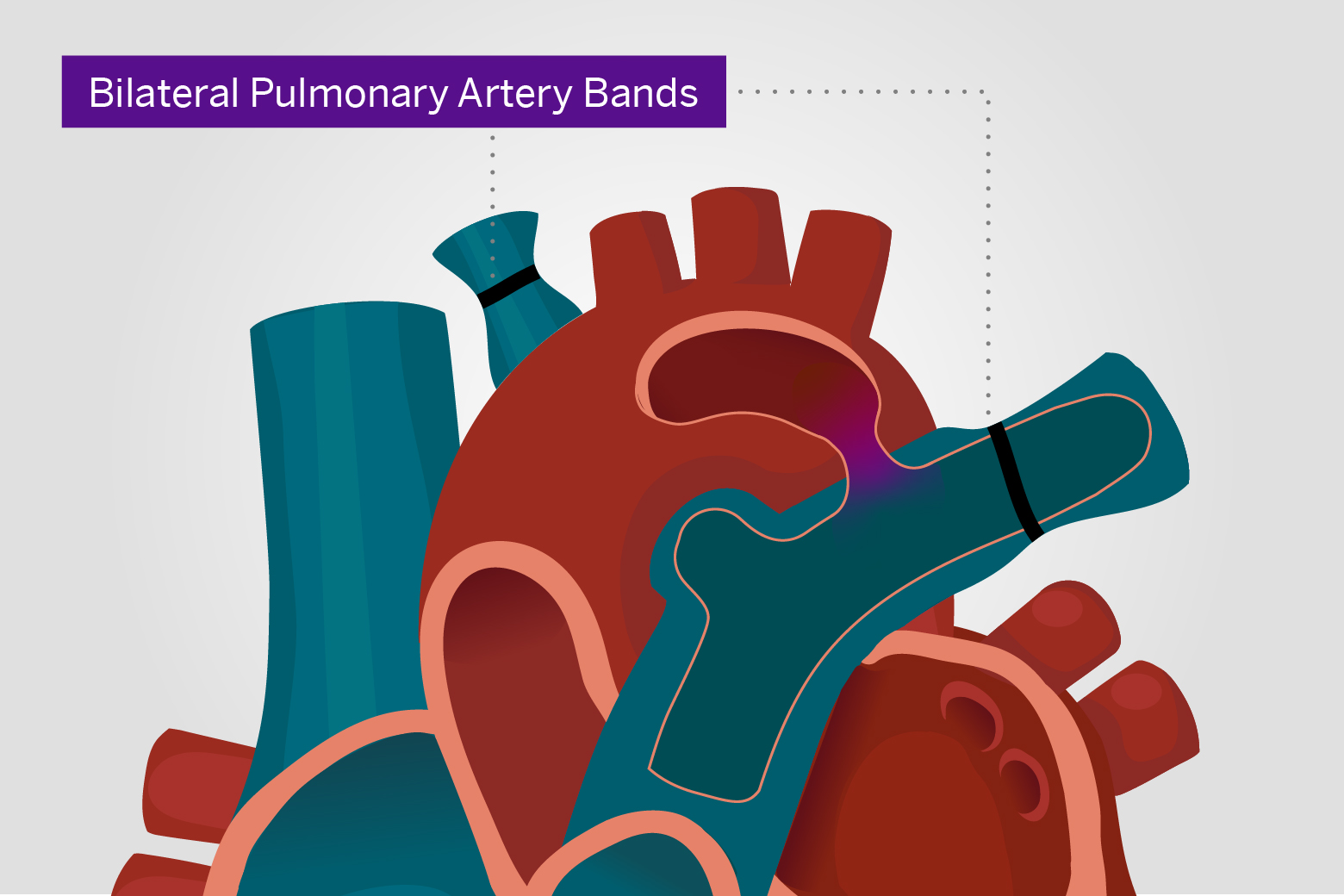
To accomplish that, intravenous prostaglandin E1 kept the newborn’s patent ductus arteriosus (PDA) blood vessel open. Surgeons also performed bilateral branch pulmonary artery banding to limit that artery’s blood flow and reduce the risk of long-term lung damage.
The baby soon stabilized and remained on a ventilator under mild sedation. At two months of life, his PDA began to constrict, requiring catheter stent implantation across the ductus arteriosus. In June 2023, a donor heart became available, allowing surgeons led by Dr. Kumar and Ralph S. Mosca, MD, to rebuild the baby’s pulmonary arteries and perform a heart transplant.
“The donor heart worked perfectly from the moment it started beating,” Dr. Kumar says. “This excellent outcome is the result of our team’s extensive experience and seamless collaboration,” adds Dr. Mosca.
“Infants who make it to transplant have a greater than 50 percent chance of doing well with the same heart 25 years later.”
Rakesh Singh, MD
The boy’s parents, who had relocated to New York, took their son home two months later, and he continued to receive extensive outpatient pediatric rehabilitation services through Rusk Rehabilitation. “Infants who make it to transplant have a greater than 50 percent chance of doing well with the same heart 25 years later,” Dr. Singh says. In December 2023, the boy celebrated another big milestone: his first birthday.