A study by orthopedic surgeons at NYU Langone Health has demonstrated that a primary biceps tenodesis procedure yields better outcomes than a secondary biceps tenodesis performed after a failed SLAP (superior labrum anterior to posterior) repair.
Orthopedic surgeons commonly see SLAP tears of the shoulder secondary to trauma and associated with overuse in overhead-throwing athletes and manual workers. An arthroscopic repair of the superior glenoid labrum where the biceps originates can maintain the patient’s anatomy, but the continued pull of the biceps on the labrum and other potential limitations have yielded a high rate of clinical failure after SLAP repair, especially among older patients.
Many surgeons have traditionally reasoned that a failed SLAP repair could be revised with little or no harm to the patient by following up with a biceps tenodesis, which has a higher success rate but requires cutting the biceps and switching its anchor from the labrum to the upper part of the humerus.
“Starting with the SLAP repair is not without harm; patients may be compromising their potential outcome more than if they just had the primary bicep tenodesis to begin with.”
Laith M. Jazrawi, MD
“Doing what we call the potentially ‘safer surgery’ by repairing it is not necessarily safer, it’s just that surgeons are more comfortable with that,” says study coauthor Laith M. Jazrawi, MD, chief of the Division of Sports Medicine. Because a biceps tenodesis involves cutting the biceps and transferring it, patients and doctors often view it as a much more involved procedure.
“In this study, we found that it’s better to do the primary biceps tenodesis, if it’s indicated, than to repair the SLAP tear,” Dr. Jazrawi says. “Starting with the SLAP repair is not without harm; patients may be compromising their potential outcome more than if they just had the primary bicep tenodesis to begin with.”
Better Outcomes
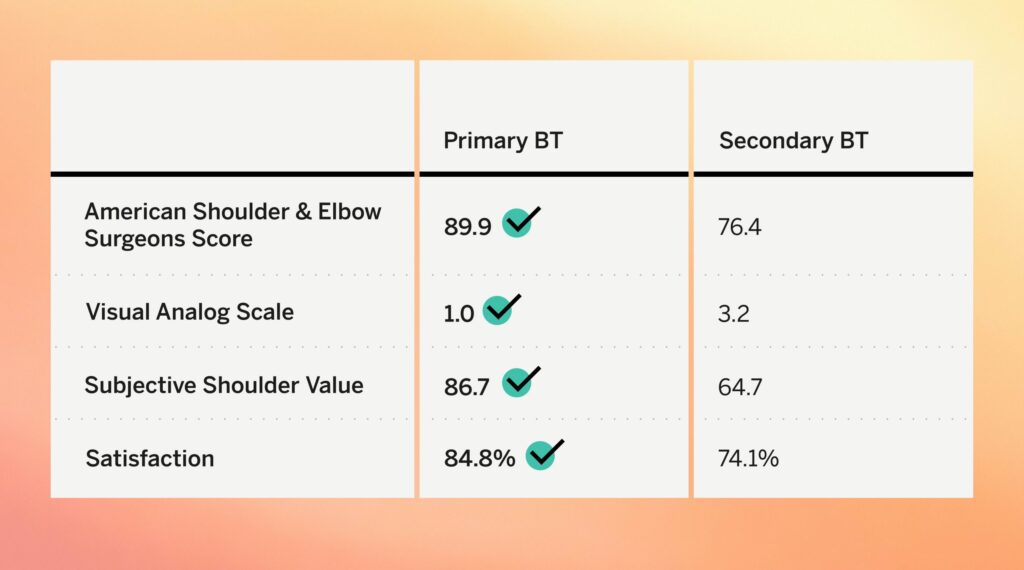
The retrospective comparison study, published in Arthroscopy, Sports Medicine, and Rehabilitation, compared 57 male patients who underwent a primary biceps tenodesis with 19 counterparts who underwent a secondary biceps tenodesis after an initial, failed SLAP repair.
The researchers found that the primary biceps tenodesis cohort reported significantly better functional and pain outcomes (Figure 1). The study found no significant differences in the rate or timing of return to play, and none of the patients required a further shoulder surgery after the biceps tenodesis.
In prior head-to-head comparison studies, a primary biceps tenodesis delivered better long-term outcomes, an easier recovery, higher patient satisfaction, and a higher return to play rate than a primary SLAP repair. The new study confirms those earlier findings in a larger, independent patient population.
“Go right after the pathology with the correct treatment from the get-go, and the current data supports that the correct treatment is a biceps tenodesis.”
Eric J. Strauss, MD
“The source of the trouble with a SLAP tear is likely the displacement of the superior labrum by the long head of the biceps,” says study coauthor and orthopedic surgeon Eric J. Strauss, MD. “If you take the long head of the biceps out of the equation and move it to a different spot, which is what a tenodesis accomplishes, you can significantly improve a patient’s symptoms because you’re basically taking away the pain generator and a lot of the theoretical reasons why a SLAP repair would fail.”
Dr. Strauss maintains that the accumulating data support a phase-out of SLAP repairs.
“One of the big take-home messages from our study and all of our research into patients with SLAP tears is take the middleman out of the picture,” he says. “While we did show that you can have a successful result after a failed SLAP repair, go right after the pathology with the correct treatment from the get-go, and the current data supports that the correct treatment is a biceps tenodesis.”