The ventricular assist device (VAD), initially used as a rescue therapy for adults with cardiogenic shock, is now proving to be useful as an adjunct to coronary artery bypass grafting (CABG) in a subset of patients with advanced heart failure.
Cardiothoracic surgeon Elias A. Zias, MD, director of NYU Langone Health’s Coronary Artery Bypass Program, pioneered an innovative technique that utilizes the device in patients with advanced-stage heart failure currently considered ineligible for traditional bypass surgery. The method uses a temporary VAD to aid recovery and improve outcomes following CABG, lowering the risk of bypass surgery for patients who, otherwise, have limited treatment options aside from transplant.
“This procedure has the potential to transform the lives of patients with advanced heart failure.”
Elias A. Zias, MD
“This procedure has the potential to transform the lives of patients with advanced heart failure by delaying the need for a heart transplant or by offering a path to recovery with bypass surgery,” says Dr. Zias.
VAD for Temporary Support
In general, patients with heart failure and an ejection fraction at or below 35 percent are at high risk for death or complications with bypass surgery, Dr. Zias says. Research suggests that reduced ejection fraction more than doubles the risk of early mortality after CABG.
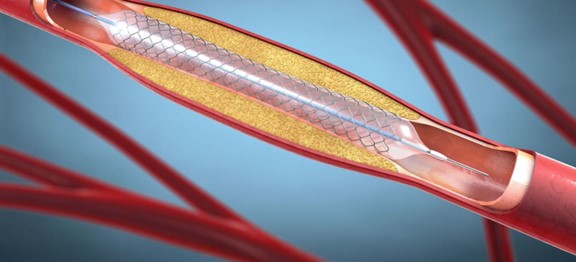
This paradigm has started to shift, however, with the availability of temporary VADs, he notes. While early versions of these devices were bulky and cumbersome to remove, modern versions can be taken out directly at the bedside with no additional anesthesia or surgery.
After coronary bypass surgery, the device is placed centrally into the aorta to temporarily assume the pumping function of the heart, allowing it to rest, Dr. Zias explains. Within a matter of days, the device is taken out, and patients tend to recover quickly thereafter.
A Viable Option for Complex Cases
Recently, Dr. Zias and the team had a case that was uniquely complex involving a 62-year-old male patient who presented with an acute pulmonary embolism. He also had heart failure with a reduced ejection fraction of 30 percent, chronic kidney disease, diabetes, hypertension, and hyperlipidemia.
“After treating the pulmonary embolism, we knew he would require CABG surgery,” Dr. Zias says. “Given his reduced ejection fraction and comorbidities, the surgical risk was higher than average. We recommended placement of a temporary VAD.”
After completing the bypass surgery, Dr. Zias inserted the temporary VAD without any complications. Within a day after the procedure, the patient was strong enough to stand and walk. At 10 days postop, the device was removed during a bedside procedure, and the patient returned home shortly after.
“Having done over 100 of these procedures, we have conducted more than any other institution across the country.”
“The device alleviates the burden on the heart as it heals, while simultaneously allowing a patient to stand and move around sooner. Together, that makes a huge difference in their overall recovery,” Dr. Zias explains.
Being Proactive, Not Reactive
When considering CABG in the setting of advanced heart failure, Dr. Zias recommends that patients be referred as early as possible to ensure optimal short-term and long-term outcomes, emphasizing that the cardiac surgeons at NYU Langone are uniquely positioned to perform this procedure.
“Having done over 100 of these procedures, we have conducted more than any other institution across the country,” Dr. Zias says. “Due to our success, the device manufacturer is now launching a trial in this cohort of patients.”