Critical Presentation Yields Discovery of Life-Threatening Clot
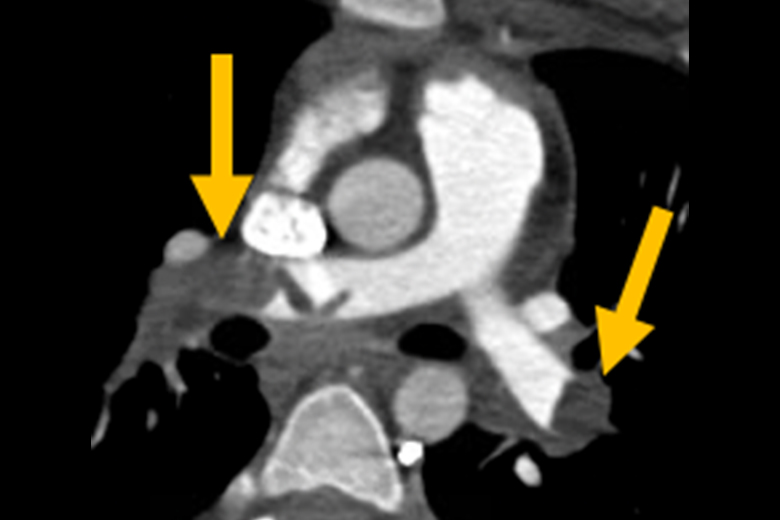
A 15-year-old girl with a family history of clotting disorders, a history of hormonal supplementation treatment for irregular menses, and recent complaints of chest pain was diagnosed with a pulmonary embolism in another hospital’s emergency department after the patient lost consciousness at home.
Though the care team immediately stabilized the patient with extracorporeal membrane oxygenation (ECMO), they were not equipped to manage ECMO in pediatric patients. Jason C. Fisher, MD, surgical director of NYU Langone Health’s Pediatric ECMO Program, was contacted to transfer the patient’s care to Hassenfeld Children’s Hospital at NYU Langone, where a multidisciplinary team mobilized.
“This case was our multidisciplinary system at work.”
Jason C. Fisher, MD
“We quickly choreographed the specialists, timing, and an operating room’s worth of equipment needed to safely transport this patient to our care,” says Dr. Fisher.
The first step was to transfer her from the other hospital’s ECMO circuit to NYU Langone’s mobile ECMO unit. “She had a near complete occlusion of cardiac output,” notes Arun Chopra, MD, director of pediatric critical care, so the team carefully titrated medications to keep the patient stable during the transfer, then managed her on the new machine until arriving safely at that Pediatric Intensive Care Unit.
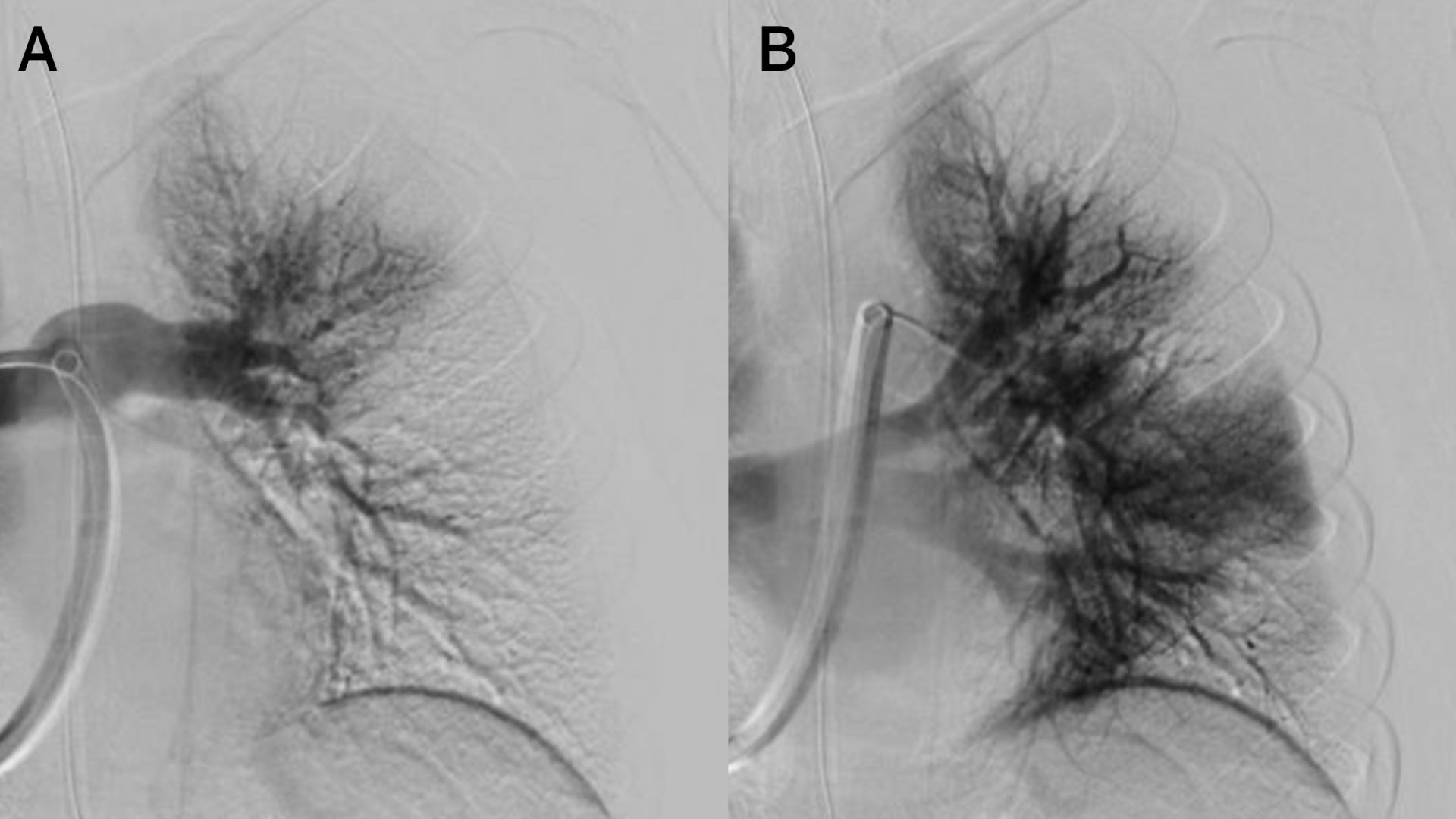
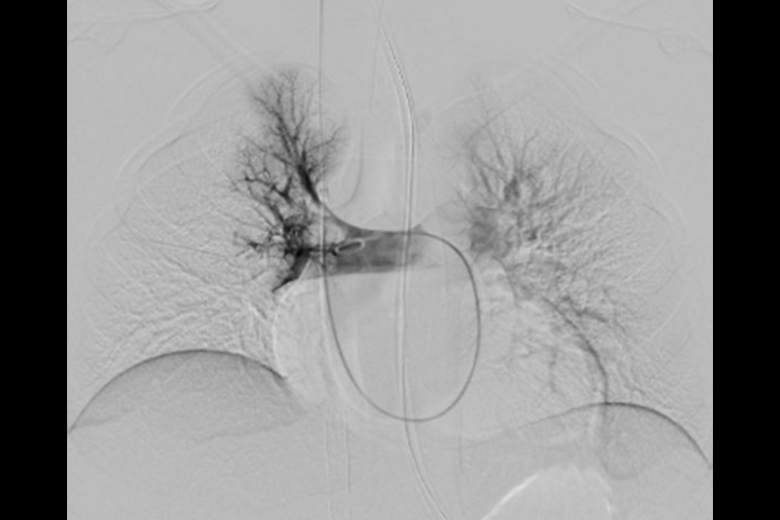
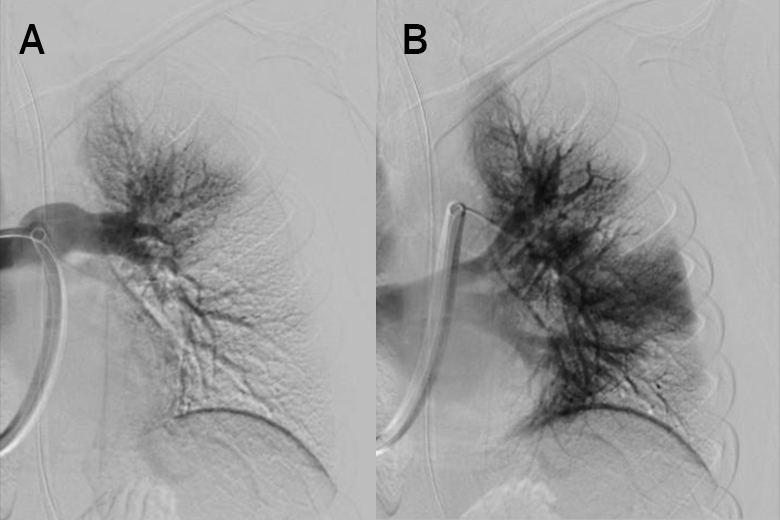
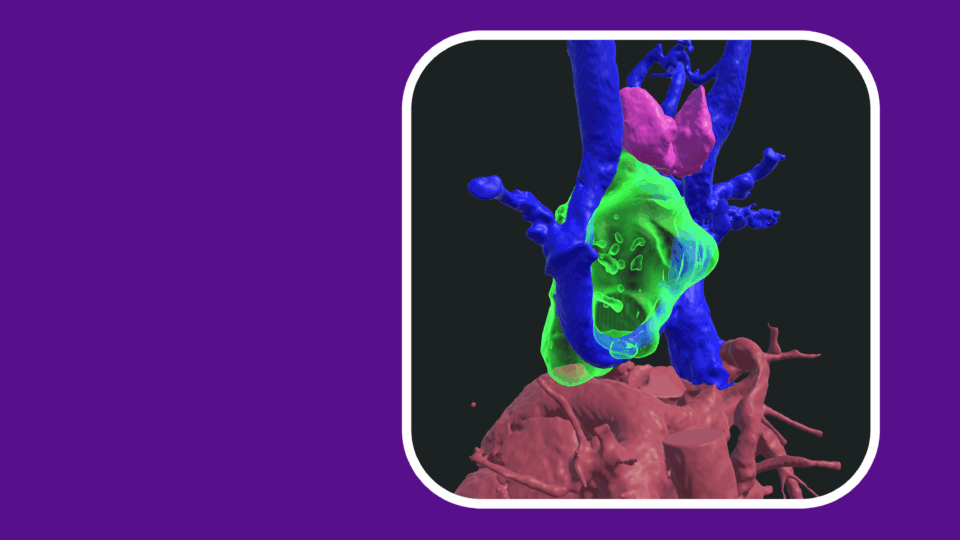
There, Frederic J. Bertino, MD, director of pediatric interventional radiology, planned endovascular treatment of the emboli. When further imaging revealed blood vessel damage and bleeding from the femoral artery from the initial, emergent ECMO placement—contraindicating thrombolytic treatment—Dr. Bertino elected to apply mechanical thrombectomy.
“The nuance was in ensuring we didn’t compete with the suction also created by ECMO circuitry. It required experienced, careful coordination with the perfusionist.”
Frederic J. Bertino, MD
Using the approach, rarely performed in pediatric patients, Dr. Bertino guided a flexible catheter through an incision in the patient’s neck into the pulmonary artery, using a syringe to create suction that removed the clots. “The nuance was in ensuring we didn’t compete with the suction also created by ECMO circuitry, which could introduce air embolism,” explains Dr. Bertino. “It required experienced, careful coordination with the perfusionist.”
Following further collaboration with the vascular surgery team to repair the prior vessel injury from the patient’s groin to the retroperitoneal space, the patient stabilized quickly, coming off ECMO within 24 hours of her arrival.
“This case was our multidisciplinary system at work—experienced coordination, combining our expertise in pediatric critical care and a novel interventional approach to deliver a good outcome for a critically ill patient,” says Dr. Fisher.