Traditional spine surgery requires a midline incision and dissection of muscle to expose the underlying bone. More recently, orthopedic surgeons have used tubular retractors and a microscope to perform less invasive operations, but they still require open dissection of the tissue, leading to soft tissue destruction, denervation, and longer periods of postoperative pain and recovery.
A breakthrough method debuted at NYU Langone Health in 2022, called dual portal endoscopic spine surgery, is a “game changer” for minimally invasive techniques, says Yong H. Kim, MD, director of the degenerative spine service in the Division of Spine Surgery. Like endoscopic knee surgery, it requires only two tiny incisions for a camera and surgical tools, minimizing pain and recovery times.
“The postoperative pain and discomfort that patients have described is remarkably different.”
Yong H. Kim, MD
“The postoperative pain and discomfort that patients have described is remarkably different,” Dr. Kim says.
Introducing the Endoscopic Technique
In June of 2022, Dr. Kim traveled to Korea to learn the technique firsthand from surgeons there. “That was just an unbelievable, eye-opening experience,” he says. “When I came back I said, ‘We’ve got to do this!’”
Returning to NYU Langone, Dr. Kim trained Charla R. Fischer, MD, an associate professor of orthopedic surgery. Since last August, the two have performed a few dozen endoscopic spine surgeries. So far, NYU Langone is among only a handful of centers in the United States and the only one in the New York metropolitan region offering the technique. Dr. Fischer is also one of the only female spine surgeons in the world performing the method.
Multiple Benefits for Surgeons and Patients
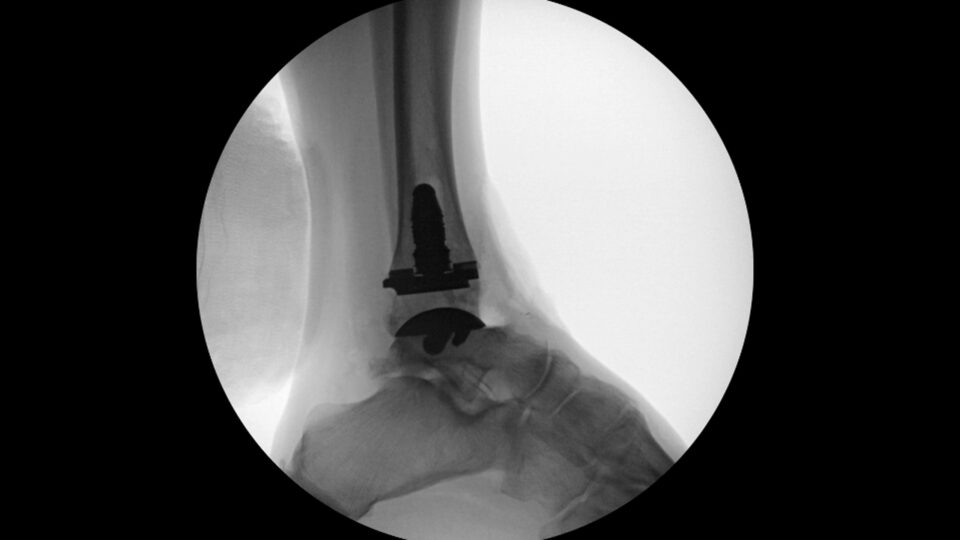
The surgical procedure begins with a 4-millimeter cut to insert a camera onto the top of the patient’s spine. A second, even smaller incision further down the back creates a working channel. “Then you triangulate and meet at the intended surgical target,” Dr. Kim says. “While the camera is illuminating the space, you can do all of the work.”
Most degenerative lumbar spine surgeries can use the technique, including discectomies, laminectomies, and fusions. As the surgeons hone their skills, they can apply it to the thoracic and cervical spine as well, Dr. Kim says.
“Our goal is to do the same surgical procedures in the spine, but with smaller access to the area and less tissue disruption and muscle and bone resection on the way,” Dr. Fischer says.
“I think as patients learn about this particular technique, they’re going to start asking about it because the outcomes are so good.”
Charla R. Fischer, MD
The method’s flexibility provides a better ergonomic option for surgeons and allows them to more easily see across the spine. Because the surgery requires only a minimal closure of skin and not muscle fascia, the procedure time can be reduced as well. Dr. Kim adds that the capital investment is considerably less than that required for conventional endoscopic surgery. “This technique utilizes everything that we already have, such as arthroscopic equipment that we use for knee and shoulder surgeries,” he says.
For patients, an additional benefit is a lessened need for postsurgical narcotics and an accompanying reduction in the risk of side effects such as drowsiness and constipation. “You don’t have that additive effect of issues related to the narcotic use,” Dr. Fischer says.
“I think as patients learn about this particular technique, they’re going to start asking about it because the outcomes are so good,” she adds.
New Opportunities for Collaboration
Conducting the new surgery at the main medical center gives the surgeons access to additional tools used by a range of other specialists, Dr. Fischer says. Likewise, nurses in different services provide valuable input about tools and techniques.
“If we had been at the orthopedic hospital, it would’ve been easy to use the arthroscopy tools like a knee and shoulder scope,” she says. “But we’re at the main medical center, where everyone’s pioneering at the next level. It was really fun to see and learn what other surgical specialties are doing.”
Beyond training NYU Langone’s five orthopedic fellows, the Department of Orthopedic Surgery plans to host an annual cadaver lab to teach other surgeons in the region and meet the growing demand. Colleagues in the Department of Neurosurgery have expressed interest as well.
“The Korean surgeons made this technique really good,” Dr. Kim says. “We want to try to make it even more innovative.”