Three Surgeons Collaborate to Repair Rare Traumatic Cloaca
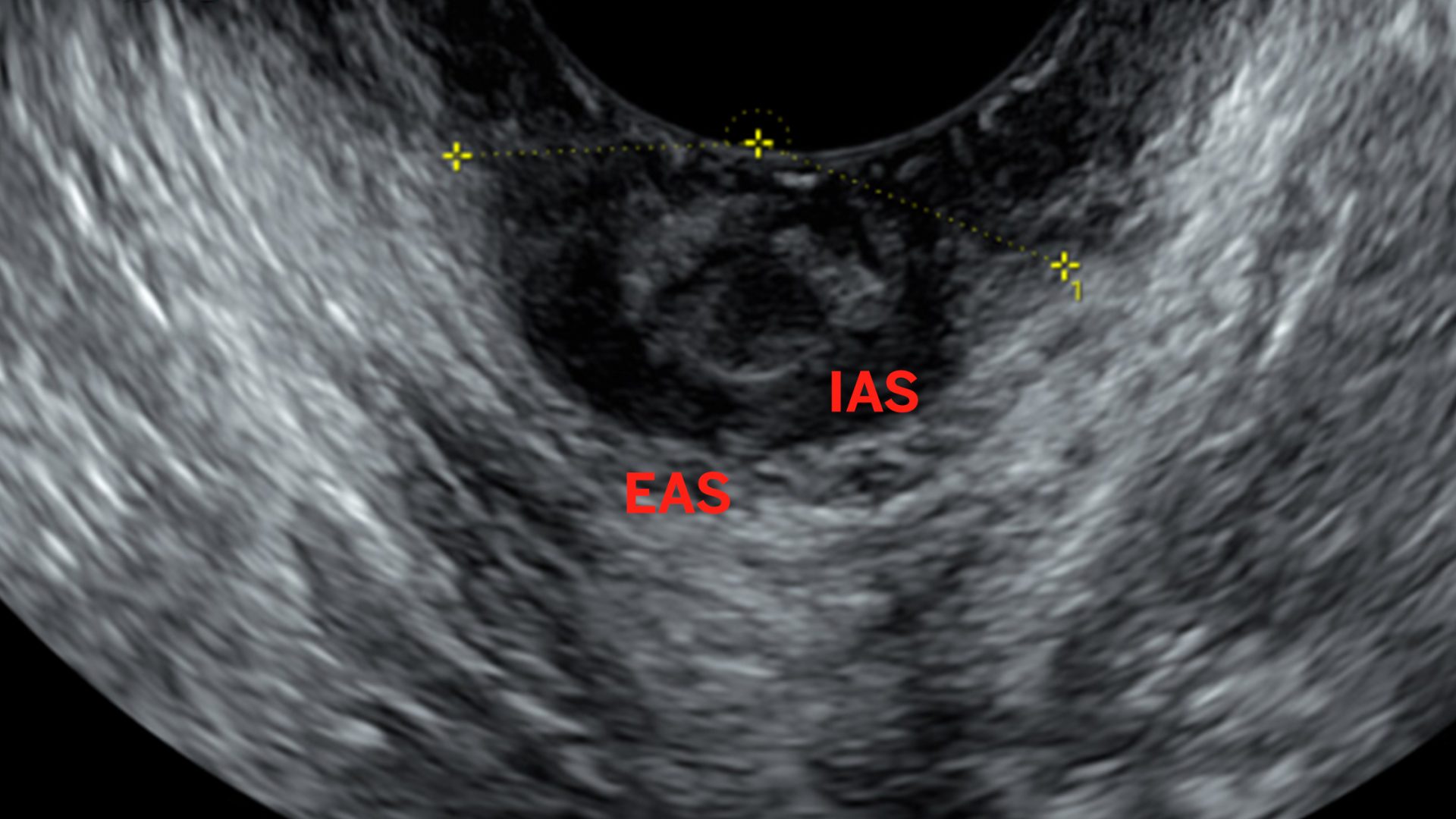
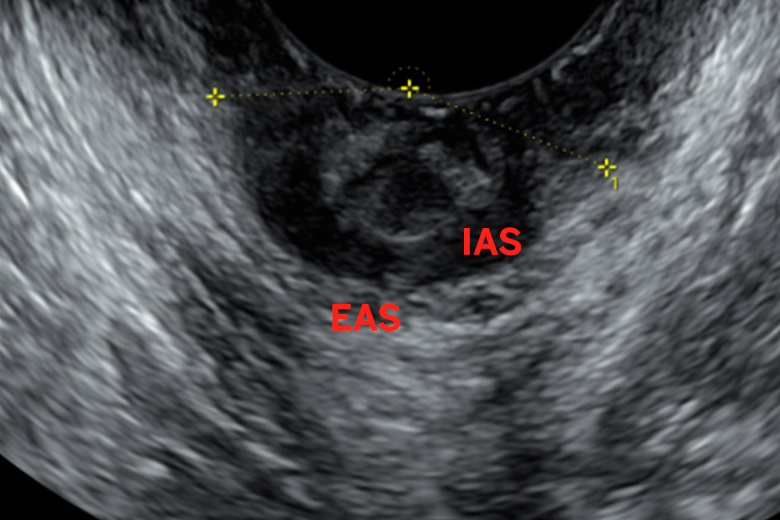
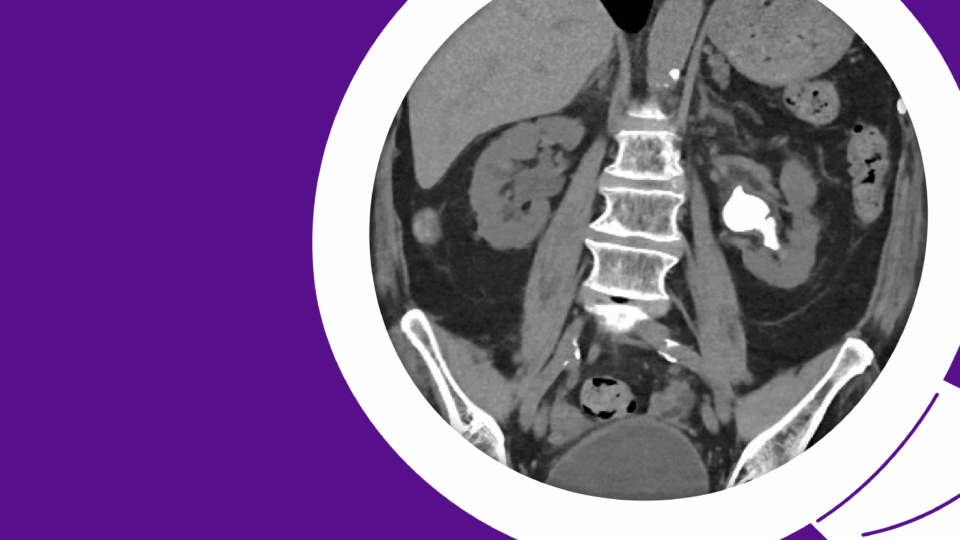
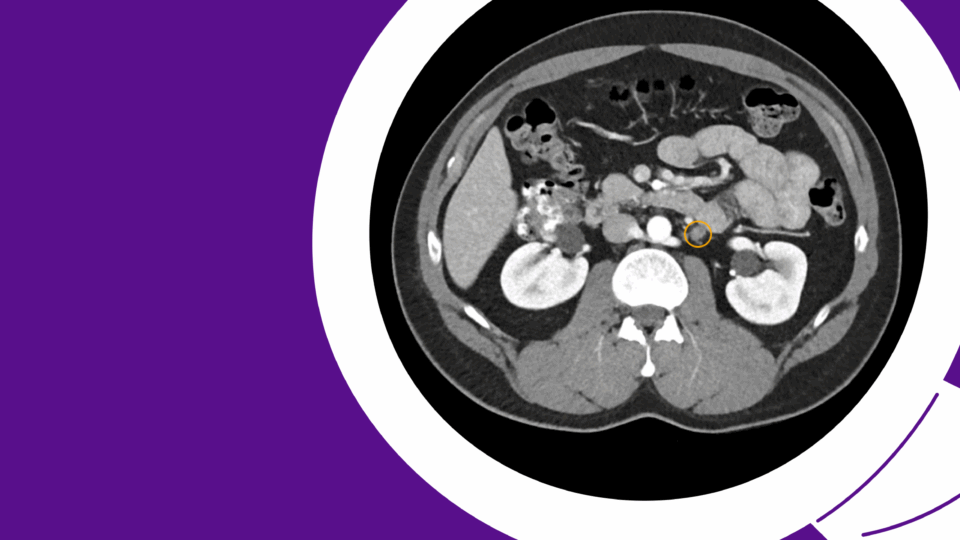
A woman in her 40s presented with fecal incontinence subsequent to a fourth-degree laceration during vaginal delivery in her home country. The patient had seen several providers without relief prior to travel to the United States, where she was referred for urogynecology consultation with Christina M. Escobar, MD. Examination revealed an open defect in the perineal body, anal sphincter complex, and rectovaginal septum, with no rectal tone.
Traumatic cloaca is a rare presentation, as precipitating injury is typically repaired during childbirth. The condition creates a single cavity involving the rectum and vagina, severely disrupting patient quality of life.
“Because it’s so rare, providers often don’t diagnose traumatic cloaca, or may be unsure where to refer patients, leaving women suffering from fecal incontinence,” Dr. Escobar says. “This patient had gone from consults with gynecologists to a colorectal surgeon to urogynecology, but we brought all three specialties together to restore her anatomy.”
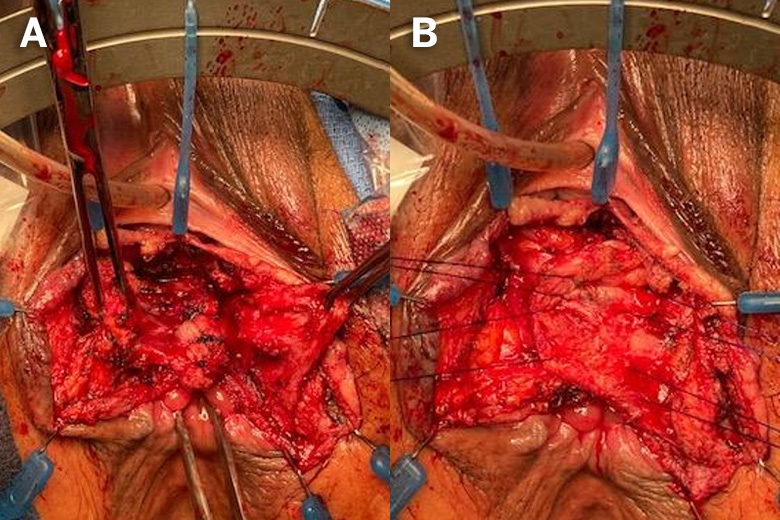
To plan the reconstruction, Dr. Escobar collaborated with NYU Langone Health colleagues Nirit Rosenblum, MD, a specialist in female pelvic medicine and reconstruction, and Marsha A. Harris, MD, a colorectal surgeon with pelvic floor expertise. Dr. Harris takes a special interest in women’s health, frequently partnering with colleagues in gynecology and urology to repair pelvic floor dysfunction.
“By pooling our pelvic floor expertise, our team expanded our toolbox three-fold and dramatically improved the patient’s quality of life.”
Christina Escobar, MD
The approach involved dissection of the rectovaginal septum and sphincteroplasty; multidisciplinary collaboration was critical to identifying, isolating, and repositioning the structures. “There is a major advantage to having a urologist, gynecologist, and colorectal surgeon side-by-side working on these adjacent areas,” says Dr. Rosenblum.
Following overnight observation, the patient was released with a care plan in place.
“This is a patient who was told her problem was not fixable, who lived with fecal incontinence for 14 years,” says Dr. Escobar. “By pooling our pelvic floor expertise, our team expanded our toolbox three-fold and dramatically improved the patient’s quality of life.”