A Spontaneous Subluxation
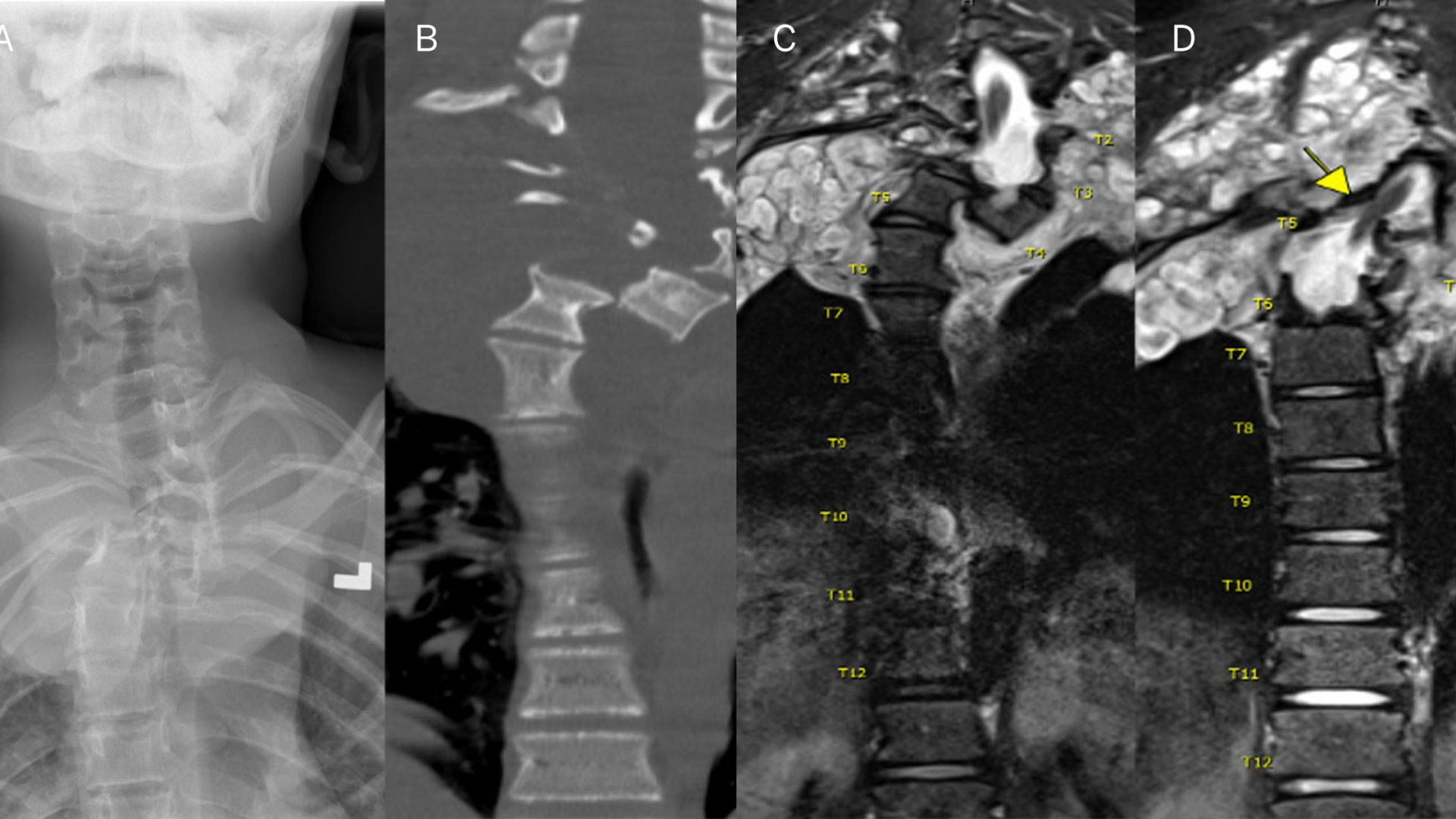
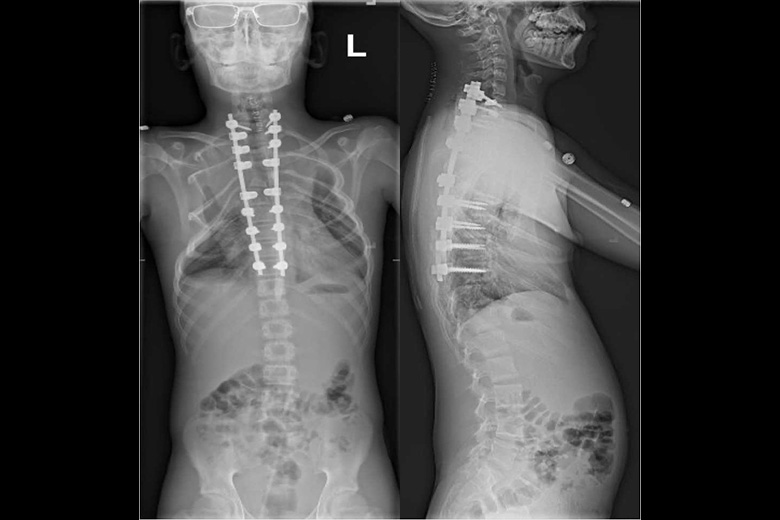
When a 17-year-old, neurologically normal male patient diagnosed with neurofibromatosis type 1 (NF1) and scoliosis experienced an extremely rare complication—a complete spontaneous lateral subluxation of his T4 and T5 vertebrae, dislocating the spine and compressing the spinal cord—a carefully planned intervention leveraging the most advanced surgical techniques and intraoperative imaging offered hope of restored mobility and a return to sports.
The young male had been followed for his scoliosis and was an established patient at NYU Langone Health’s Comprehensive Neurofibromatosis Center. With the sudden and atypical spinal dislocation, he was referred to Darryl Lau, MD, an assistant professor of neurosurgery and director of complex spine and spinal deformity at NYU Langone. Dr. Lau confirmed that for such a high degree of spinal instability and spinal cord compression, intervention was urgent to preserve the patient’s neurologic function.
“In NF1 and dystrophic scoliosis, spontaneous subluxation can occur in cases where the disease has progressed severely. . . . [S]uch complex disease involving tumor, spinal cord injury, and scoliosis becomes a case for neurosurgery.”
Darryl Lau, MD
“In NF1 and dystrophic scoliosis, spontaneous subluxation can occur in cases where the disease has progressed severely. Combination of tumor growth, dural ectasia, and likely other unknown factors result in bony changes leading to instability,” Dr. Lau explains. “You would rarely see this severe of a fracture even with trauma, and such complex disease involving tumor, spinal cord injury, and scoliosis becomes a case for neurosurgery.”
A Rare Case for Surgery
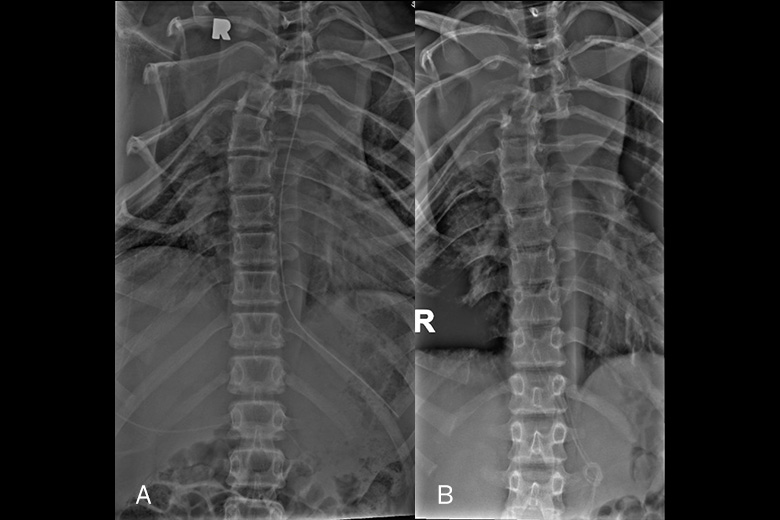
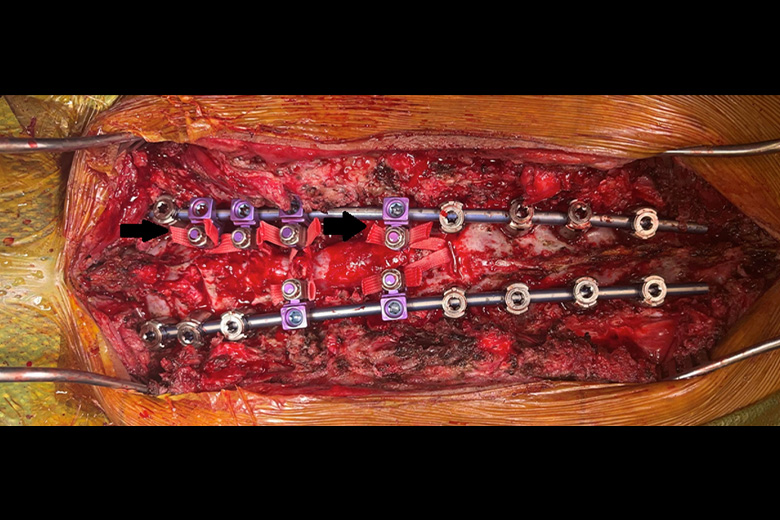
Surgical treatment for NF1 dystrophic scoliosis is extremely challenging due to abnormal bony anatomy (inability to gain adequate spinal fixation), dural ectasia resulting in cerebrospinal fluid leak, and the need for tumor resection. After first attempting to realign the spine through halo gravity traction and seeing only minimal reduction in vertebral translocation, Dr. Lau and a multidisciplinary team planned a multilevel vertebral body resection and spinal reconstruction.
While resection of the widespread tumor tissue typically observed in NF1 is not a primary goal of these procedures, notes Dr. Lau, significant resection was needed simply to enable the approach to this patient’s spine.
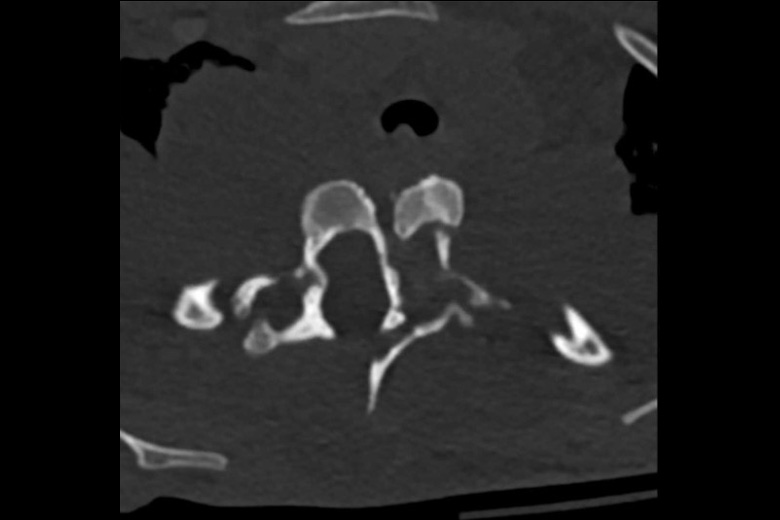
Due to the volume of tumor tissue in the thoracic spine, which had thinned out the ribs and vertebral bodies and likely contributed to the translocation, the surgical team had to forego pedicle screws and instead employed a traditional method of laminar banding to the spine. The intricate spacing of screws would have been impossible without NYU Langone’s advanced intraoperative CT and navigation systems, notes Dr. Lau.
Although vertebral column resections are typically reserved for the most severe deformities as this technique involves intricate work around the spinal cord and nerves, in this case both T4 and T5 were removed to facilitate complete reduction and achieve alignment.
Improving Patient Outcomes
Patients with NF1 having complex spinal reconstructions need to be carefully monitored for pseudarthrosis and mechanical failure years down the line, but this patient is recovering well, says Dr. Lau. His team’s combination of ever-expanding surgical expertise and new intraoperative technologies is allowing the Comprehensive Neurofibromatosis Center to take on a growing number of patients whose complex scoliosis, spinal tumors, and their concomitant effects would have once been inoperable, he notes.