While revision cochlear implant (CI) surgery has been relatively uncommon, occurring at rates ranging from 4 to 10 percent, it can be expected to increase in importance as more devices implanted over the past several decades age into failure. The most common indication is hard failure, but soft failures, infection and wound complications, improper initial placement, and electrode migration or extrusion can also require a revision procedure.
“These are man-made devices, so the electronics can fail for various reasons. We are often talking about devices that were placed 30 or 40 years ago,” says Daniel Jethanamest, MD, director of the Division of Otology, Neurotology, and Skull Base Surgery in NYU Langone Health’s Department of Otolaryngology—Head and Neck Surgery.
Experts in the Cochlear Implant Center at NYU Langone Health have been performing revision surgery for decades. In a recent retrospective review of revision CI surgeries at the center (publication forthcoming), they found that the revision procedures led to similar clinical outcomes as the original implants.
They reviewed 100 surgeries in 83 patients from 2011 to 2020. When available, intraoperative X-rays were independently reviewed by an experienced otologist to determine angular depth of insertion of the CI electrode.
“Once you remove the very thin electrode, one challenge is to ensure we get a new device back into that one tiny opening again—the scar tissue must be cleared away.”
Daniel Jethanamest, MD
“One of the concerns in these revisions is that there may be significant fibrosis. Once you remove the very thin electrode, one challenge is to ensure we get a new device back into that one tiny opening again—the scar tissue must be cleared away,” Dr. Jethanamest says. “We wanted to examine our surgery characteristics and evaluate the outcomes.”
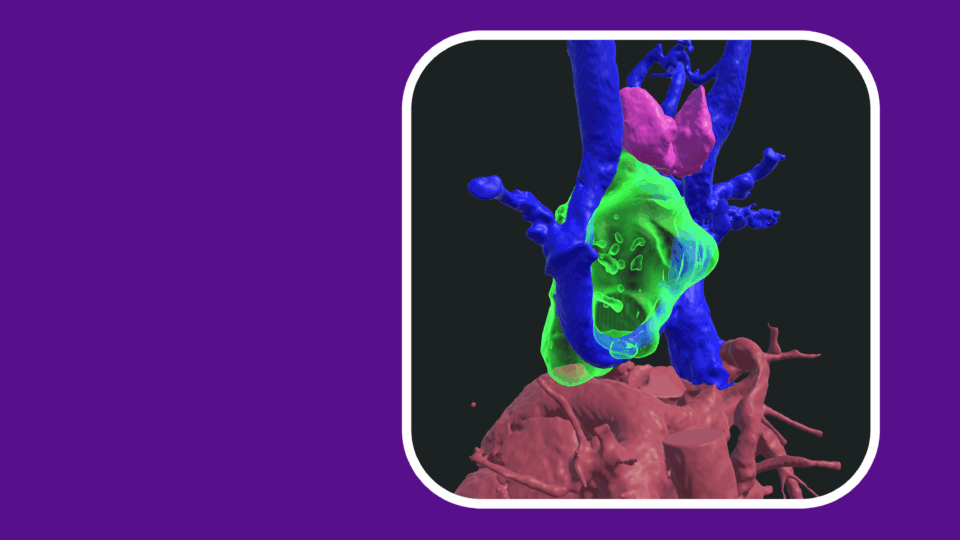
Importance of Surgical Imaging
The center’s unique approach to surgical imaging developed over the years has been essential to its success with revision procedures, Dr. Jethanamest explains.
“We take X-rays of the cochlear implant while we’re still in surgery. We try to capture the implant and its coil to ensure it is in the right position and it’s holding the right shape. Based on those X-rays, we can use a technique to calculate the angular insertion depth.”
Before surgery, the surgical team establishes a comprehensive plan including technique, the best approach, and the appropriate device.
“We have to remove the original device safely to ensure we don’t encounter any issues with local structures. Once we’ve replaced the electrode, we perform that X-ray and neurophysiologic tests to confirm that the implant is in position.”
Choosing Replacement Implants
Additionally, the team has found there are nuances in choosing a new CI device for revision surgery, notes Dr. Jethanamest.
“We try to match up a modern device with one that has been working well, and we take care to think about the dimensions of contemporary electrodes and how they will fit in the existing spaces. The patient’s brain has adapted to a particular device, sometimes since childhood. Is it easy to do it again many years later? We don’t know.”
“We take care to think about the dimensions of contemporary electrodes and how they will fit in the existing spaces.”
Much of the new technology comes in the external pieces, Dr. Jethanamest says, and the manufacturers typically support their legacy devices.
“For the most part, replacing a device with something similar seems to work out well, even if there is brand new technology and programming algorithms with the newer devices. Surgically, finding the right size and fit and getting the electrode back into position is our main goal.”
Planning for an Increase in Patient Needs
Dr. Jethanamest and his team aim to catalogue and review the different types of electrodes and how they perform over time, including new devices that continually become smaller and smarter.
“For now, they are around 1 millimeter in diameter,” he says. “The question is, someday, when one of the slim ones fails, will we have even slimmer ones or different form factors altogether? Maybe something a little more rigid would help, but the flexible ones work as long as you can get the right anatomic exposure.”
The researchers have also just completed a study, collaborating with colleagues in radiology, to evaluate a protocol for optimizing image quality and reducing the associated artifact of MRI in patients with CIs.