Surgery for adult spinal deformities carries a high rate of intra- and postoperative complications, reoperations, and readmissions. A retrospective cohort study of 263 adult patients led by researchers at NYU Langone Health’s Spine Center found that implementing a preoperative multidisciplinary conference to discuss high-risk cases led to striking gains in multiple quality and safety metrics.
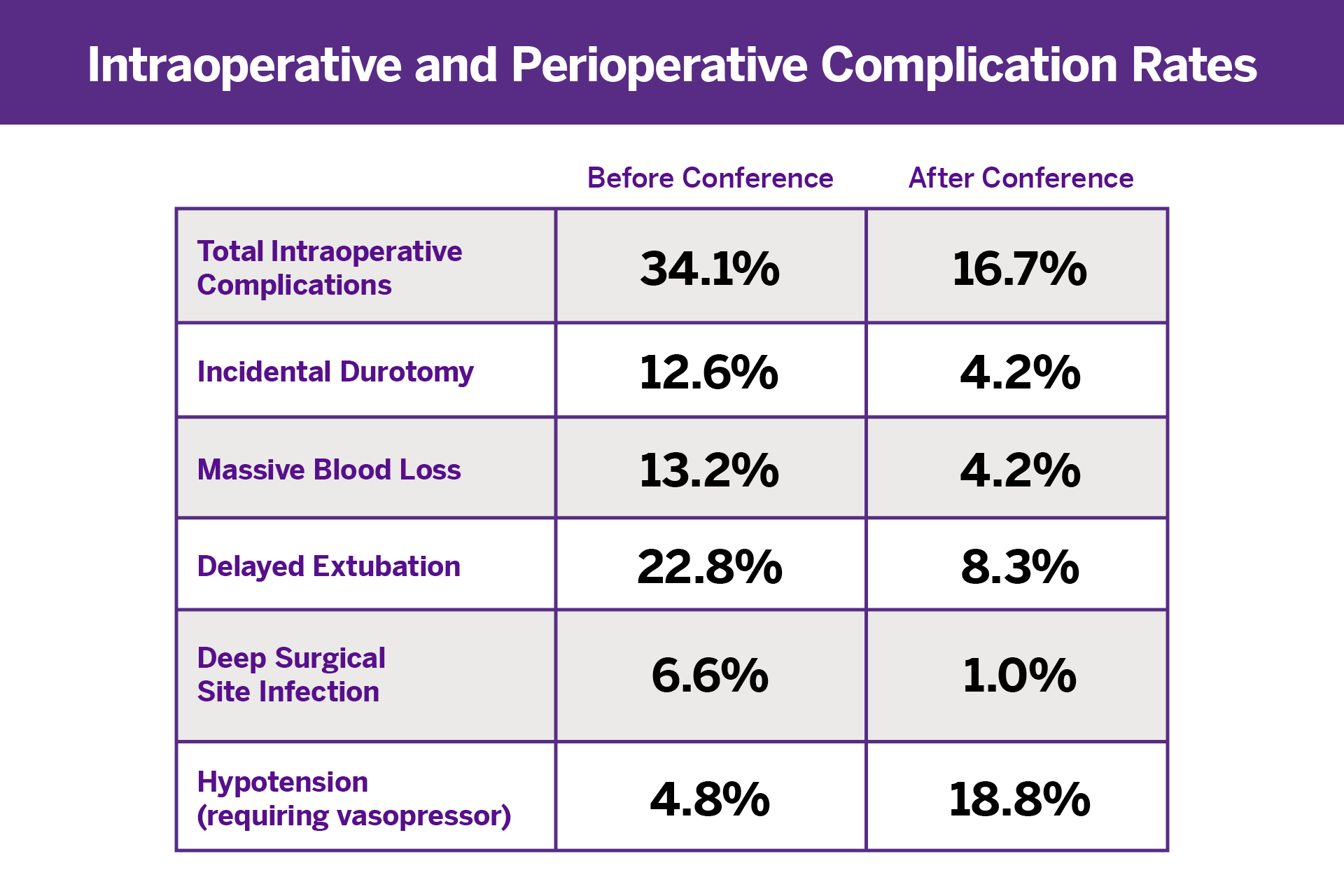
The conference, added to the weekly spine surgery indications conference starting in February 2019, included experts in orthopedic spine surgery, neurosurgery spine, anesthesia, intraoperative monitoring neurology, and neurological intensive care. Compared to 167 consecutive patient cases before the launch of the conference, 96 post-conference cases showed a significant decrease in total intraoperative complications, massive blood loss, incidental durotomy, delayed extubation, and deep surgical site infections.
One exception to the overall improvement in complications was an increase in hypotensive episodes requiring vasopressors, a finding the researchers say could be attributable to the higher average age of patients in the post-conference group but one that did not lead to a longer length of stay or higher readmission rate.
The multidisciplinary conference, in fact, yielded a statistically significant decrease in reoperation and readmission rates at both 30 and 90 days. Those gains may be attributable to appropriate patient selection and optimization of the surgical plan, according to study co-author Charla R. Fischer, MD, associate professor of orthopedic surgery. “Spinal deformity surgery is one of the most complicated and high-risk operations in our field,” Dr. Fischer says. “This single-center study shows how impactful multidisciplinary conferences are before high-risk, complex spinal deformity surgeries. It’s critical for institutions to develop this protocol to achieve the best outcomes for their patients.”
“This single-center study shows how impactful multidisciplinary conferences are before high-risk, complex spinal deformity surgeries. It’s critical for institutions to develop this protocol to achieve the best outcomes for their patients.”
Charla R. Fischer, MD