Cindy L. Bredefeld, DO, is a clinician and trial director with a focus on diabetes and lipid disorders. Here, she discusses hypobetalipoproteinemia disorders—conditions with low or absent lipid levels, which impair the normal absorption and transport of fats and fat-soluble vitamins. Working with Mahmood Hussain, PhD, Dr. Bredefeld has helped to create a classification system for these disorders, and advocates for awareness and research through the Abetalipoproteinemia and Related Disorders Foundation.
Physician Focus: Your lipid disorders research includes low lipid conditions—less recognized than hyperlipidemia, which leads to coronary artery disease. Describe these less common disorders.
Dr. Bredefeld: Low-lipid disorders are collectively recognized as familial hypobetalipoproteinemia. They are monogenic, with a number of known genetic mutations that determine the phenotype and disease progression.
Recently, Dr. Hussain and I co-authored a consensus guidance that classifies these disorders into two categories. Class II disorders are due to enhanced catabolism of lipoproteins and are typically asymptomatic; in fact, these mutations can be beneficial in preventing cardiovascular disease.
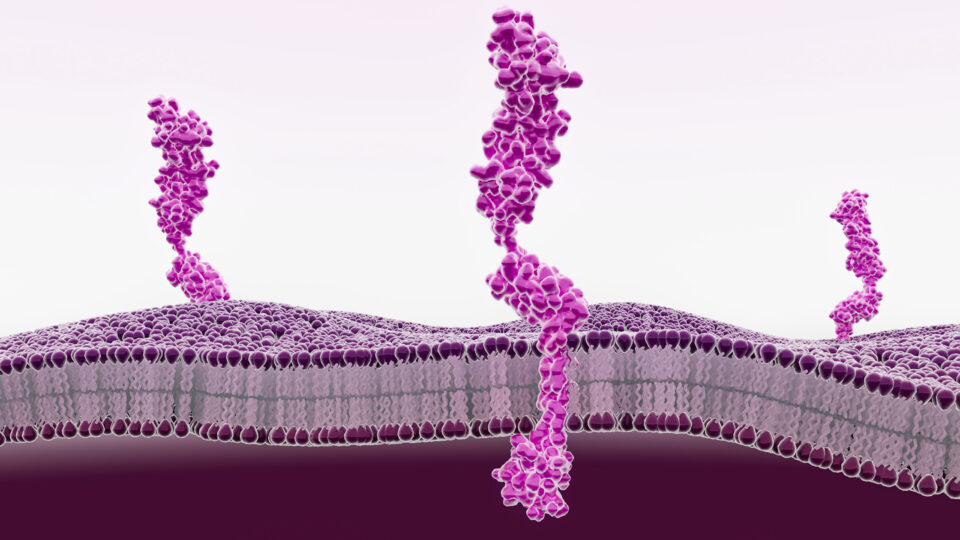
On the other hand, class I conditions—including abetalipoproteinemia, hypobetalipoproteinemia, and chylomicron retention disease—are severe. They inhibit the assembly and secretion of lipoproteins, so lipids become trapped in the liver and intestine leading to symptoms of steatosis and fat malabsorption. Without fat-soluble vitamins reaching target tissues, patients often suffer from blindness, peripheral neuropathy, and hemorrhage.
Advancing Diagnosis, Treatment and Research
Physician Focus: How are low-lipid disorders diagnosed and treated in children or adults?
Dr. Bredefeld: These are ultra-rare disorders that are usually identified after an arduous diagnostic journey. Parents may notice symptoms of fat malabsorption—their babies do better when they restrict fats, such as in breast milk. A pediatric gastroenterologist might order a workup for malabsorption. If a lipid panel is obtained during this evaluation, it clinches the diagnosis. Genetic testing can confirm the diagnosis.
Patients require lifelong management with megadoses of fat-soluble vitamins. Additionally, there are important dietary concerns; fats must be restricted to just five—the amount in one large egg—to 15 grams per day.
“These are ultra-rare disorders that are usually identified after an arduous diagnostic journey.”
Cindy L. Bredefeld, DO
Physician Focus: You helped launch the Abetalipoproteinemia and Related Disorders Foundation. What is the foundation doing to advance understanding of these disorders?
Dr. Bredefeld: First and foremost, we are engaged in advocacy to increase awareness. There is a general lack of understanding regarding the management of these disorders, particularly among insurance companies. They can be reluctant to cover the cost of these “vitamins”—which can average $800 per month out of pocket—because they’re not seen as the critical treatments they are. Insurers may not understand that a baby could hemorrhage, or that an adult patient could develop severe neuropathy or blindness. We have provided letters of medical support for physicians to submit to insurers.
Dr. Hussain, the foundation’s president, is a basic researcher while I’m on the clinical side. We integrate the two and bring patients, caregivers, physicians and researchers together to meet an unmet clinical need for these rare disorders. We have assembled an international forum across seven countries to create an expert consensus around the diagnosis and management of hypobetalipoproteinemia.
Physician Focus: Are you also involved with research on the other side of lipid disorders, hyperlipidemia?
Dr. Bredefeld: Yes. Some of the research in hypolipidemia is informing our understanding of how to manage hyperlipidemia. Several of the genes implicated in class II hypolipidemia have inspired currently available treatments for disorders on the opposite side of the spectrum, such as familial hypercholesterolemia, but also for patients with coronary artery disease to help reduce their risk of cardiac events.
I am the principal investigator for a clinical trial investigating ANPTL3 monoclonal antibody for severe hypertriglyceridemia, a common lipid condition—another example of how research in rarer disorders can benefit the larger patient population.
Transferring Insights to More Common Conditions
Physician Focus: Why do you feel it’s so important to support research and treatment of these rare diseases?
Dr. Bredefeld: As I mentioned, understanding low lipids can directly inform treatment advances for hyperlipidemia, which is highly prevalent.
In addition, for patients impacted by hypolipidemia, we’re learning more about the mechanisms of disease and potential treatment pathways. Through the foundation, we’re developing a biobank and patient registry to understand the natural history of these disorders. Another initiative is to discover novel vectors that could more efficiently deliver high-dose vitamins to patients with class I hypolipidemias. These studies could also help inform treatment of other, more commonly seen malabsorption disorders.