The neovascularization caused by retinopathy of prematurity (ROP) can sometimes be halted with drugs or laser therapy, preventing the negative sequelae and late-stage disease that can require vitrectomy surgery. In premature infants, this surgery requires precision and specialized expertise.
Vaidehi S. Dedania, MD, an assistant professor in the Department of Ophthalmology, treats both children and adults with retinal disease. However, it is her expertise in ROP surgery that attracts patients from across the New York region.
“Kids are not little adults; their eyes haven’t yet developed completely, so special considerations need to be made for surgeries unique to this group,” says Dr. Dedania. “Some of these babies are under three pounds.”
More than 40 percent of at-risk premature infants develop some stage of ROP, with approximately 12.5 percent developing severe ROP. “The median age for treatment-requiring ROP is 36 to 41 weeks,” says Dr. Dedania. “Now, we’re able to save more 22- and 23-weekers. The younger the baby, the greater the risk for developing ROP.”
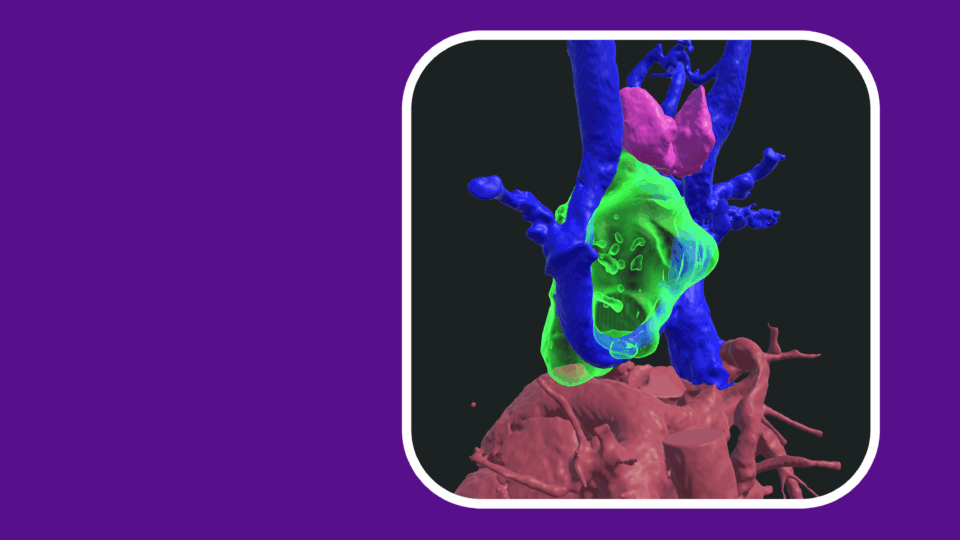
Imaging Infant Eyes
Most ROP regresses without treatment, yet for those cases that do progress, it can be difficult to predict which babies will require treatment and when. Dr. Dedania is involved in several initiatives aimed at early prediction and diagnosis of advanced disease.
“We need to find ways to better visualize intraoperatively for these babies—we’re still using all adult equipment.”
Vaidehi S. Dedania, MD
“We have advanced technology—including OCT [optical coherence tomography] and OCT angiography—that we use in diabetic retinopathy and other retinal diseases,” she says. “While we have some of this available for use in children, we have to develop a better understanding of how this technology can offer predictive data in ROP.”
In collaboration with colleagues in the Advanced Ophthalmic Imaging Laboratory, Dr. Dedania is participating in a single-center study to characterize and evaluate retinal pathologies using OCT.
“Additionally, we need to find ways to better visualize intraoperatively for these babies—we’re still using all adult equipment,” she says.
The Role of Biomarkers
Dr. Dedania says biomarkers with high sensitivity and specificity are needed to predict ROP. “We use biomarkers from tears and blood—less-invasive means—to obtain the metrics. But we really need to understand how to utilize this information,” she notes.
To help address this question, Dr. Dedania and colleagues have implemented a vitreous biorepository at NYU Langone Health. “This is what we want to find out: are there vitreous biomarkers predictive of ROP and how do those correlate with biomarkers from blood or tears?”
Improving Access to Care
Lastly, Dr. Dedania believes telemedicine is an essential part of ensuring that all premature babies get screened for high-risk ROP. She participated in research that evaluated the feasibility of screening using a novel smartphone-based fundus photography device, and recently completed a study evaluating ROP screening patterns during the pandemic.
“Especially in resource-poor communities, we need to ensure that all premature infants get proper ROP screening and have access to the interventions that can prevent blindness,” she said.