A woman in her early 70s with severe degenerative mitral valve (MV) disease—in the setting of extensive mitral annular calcification (MAC)—was referred to specialists at NYU Langone Health to devise a precise surgical plan for valve replacement and MAC excision.
Echocardiography showed a regurgitation volume of 91 mL and near-circumferential MAC involving the anterior and posterior leaflet hinges and the left trigone. “The center of her heart looked like it had been turned to stone,” explains Eugene A. Grossi, MD, the Stephen B. Colvin, MD, Professor of Cardiothoracic Surgery and director of cardiac surgical research.
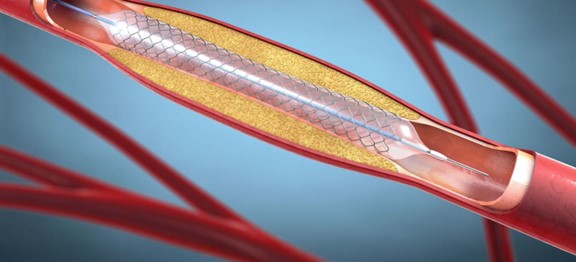
Because extensive annular calcification significantly raises the risk of perioperative complications, including atrioventricular groove disruption, paravalvular leak, and coronary artery injury, Dr. Grossi and Didier F. Loulmet, MD, chief of robotic cardiac surgery, opted for a robotic-assisted approach for its precise, controlled handling of heavily calcified tissue.
“Our totally endoscopic, robotic-assisted approach offers improved safety compared with conventional alternatives.”
Eugene A. Grossi, MD
“The mortality for these operations can be as high as 20 percent, depending on both the severity of the MAC and the surgical team’s expertise,” Dr. Grossi says. “Our totally endoscopic, robotic-assisted approach offers improved safety compared with conventional alternatives.”
A Challenging, But Successful Procedure
After discussions among the care team, it was clear that surgical intervention via sternotomy was less preferable to the fully endoscopic, robotic approach, primarily due to enhanced precision and visualization offered by the da Vinci system.
“We all agreed that the totally endoscopic approach would be preferable,” notes Dr. Loulmet. “After reviewing the preop imaging, we knew the degree of annular calcification was quite extreme—this was one of the most complex robotic mitral valve replacements we’ve ever undertaken.”
“After reviewing the preop imaging, we knew the degree of annular calcification was quite extreme—this was one of the most complex robotic mitral valve replacements we’ve ever undertaken.”
Didier F. Loulmet, MD
To achieve an optimal result, the surgical team slowly detached the calcification at the hinge of A1, P1, P2, and P3, and carefully controlled the generated debris, with the aim of removing the entirety of the annular calcium to allow for an appropriate-sized valve replacement.
Following extensive MAC resection at the hinge of A1, P1, P2, P3, and both the left trigones, ventriculoplasty repair of the atrioventricular groove was performed with a bovine pericardial patch, and both papillary muscles were re-attached to the lower edge of the patch. Subsequently, the MV was replaced with a 31-mm ELS Mitris Resilia bioprosthesis.
Ultimately, the case was codified as a Type II posterior, and the etiology was deemed degenerative (Barlow disease with four-segment MAC), extending to the leaflet tissue, the anterior papillary muscle, and the left ventricular posterior wall.
The patient had an uneventful postoperative course and was discharged to home on postoperative day three.