Since launching in summer 2023, the Pediatric Liver Transplant Program at Hassenfeld Children’s Hospital at NYU Langone has quickly earned recognition as No. 1 in New York State for outcomes. Co-led by transplant surgeon Adam Griesemer, MD, and pediatric hepatologists Debora Kogan-Liberman, MD, Nadia Ovchinsky, MD, and Jennifer M. Vittorio, MD, the program is also celebrating the recent completion their 30th pediatric liver transplant.
Here, Dr. Ovchinsky, an internationally recognized expert in liver disease and director of NYU Langone’s Division of Pediatric Gastroenterology and Hepatology, discusses the program’s initiatives, depth of specialized expertise, and collaborative care philosophies driving its results.
Physician Focus: Congratulations on this outstanding achievement. Reflecting on the past two years, what was the vision for the program and how has it evolved along the way?
Dr. Ovchinsky: From our program’s launch in 2023, we have focused on quality and safety at every step of the transplant journey: from pre-transplant care through surgery and long-term follow-up. We have steadily and strongly built the program to what it is today: a leading program in the region with the expertise to care for the most complex patients while maintaining the quality and safety standards that families expect at Hassenfeld Children’s Hospital.

Peri-transplant management has been one of the most challenging areas because a new transplant program requires constant adjustment. To support this, we hold daily multidisciplinary rounds that bring together hepatology, surgery, critical care, infectious diseases, pharmacy, and any other subspecialties essential to individualized, complex care. Our hepatologists work hand-in-hand with our surgeons and remain actively involved in the ICU postoperatively to ensure coordinated care.
“From the very beginning, we have focused on offering transplant to every patient for whom it is feasible, including the most complex and high-risk patients.”
As our program has evolved, we’ve built a pediatric hepatology service, which is a separate medical service on the floor, not just in the ICU, that provides specialized care for all patients with liver disease as well as a consultation service for all other pediatric patients in the hospital.
An aspect of our program that hasn’t changed is our approach to patient selection. From the very beginning, we have focused on offering transplant to every patient for whom it is feasible, including those with the most complex and high-risk conditions. Our living liver donor program further expands access to transplantation and allows us to offer life-saving care to children who might otherwise have limited options.
Physician Focus: What specific clinical or operational factors do you believe most directly contribute to the program’s excellent outcomes?
Dr. Ovchinsky: A central pillar is surgical director Dr. Griesemer, who brings expertise to manage the most challenging and technically-demanding cases, supported by our multidisciplinary teamwork. Our highly-coordinated efforts across medical hepatology, transplant surgery, ICU, anesthesia, nursing, social work, psychology, and a dedicated transplant pharmacist are what make our program and outcomes so strong. We build our protocols together and optimize communication with weekly multidisciplinary meetings to refine the protocols and discuss cases.
“Our highly-coordinated efforts across medical hepatology, transplant surgery, ICU, anesthesia, nursing, social work, and a dedicated transplant pharmacist are what make our program and outcomes so strong.”
Another unique strength of our program is the close collaboration with pediatric interventional radiologists, Frederic J. Bertino, MD, and Dhara Kinariwala, MD. They play a critical role in managing peri-transplant complications using minimally invasive procedures, often allowing us to resolve issues without the need for additional surgery.
Physician Focus: Sala Institute for Child and Family Centered Care is central to the holistic care provided at the hospital. How do their resources enhance the transplant patient experience?
Dr. Ovchinsky: We also owe a lot of our success to the comprehensive resources provided through Sala Institute, including a transplant social worker, nutritionist, transplant psychologist, and strong Child Life Services. These resources enhance the patient experience during complex procedures by addressing both physical and emotional needs—and doing so in a personalized way.
As an example, my first transplant evaluation at NYU Langone was a teenager, a very complex case. The first note in the patient’s chart in the ICU was not from surgery or critical care, but music therapy. When she woke after transplant, the first thing she asked for was the music therapist. That moment captured for me what Hassenfeld Children’s Hospital truly represents—a community where healing extends beyond medicine. That therapeutic aspect of comprehensive care is just not often available at other hospital systems.
Our child life specialists also continue to support patients after transplant in the outpatient clinic, which is unique. Families often tell us the hospital feels like part of their family and that Sala Institute’s resources helped them get through their toughest days.
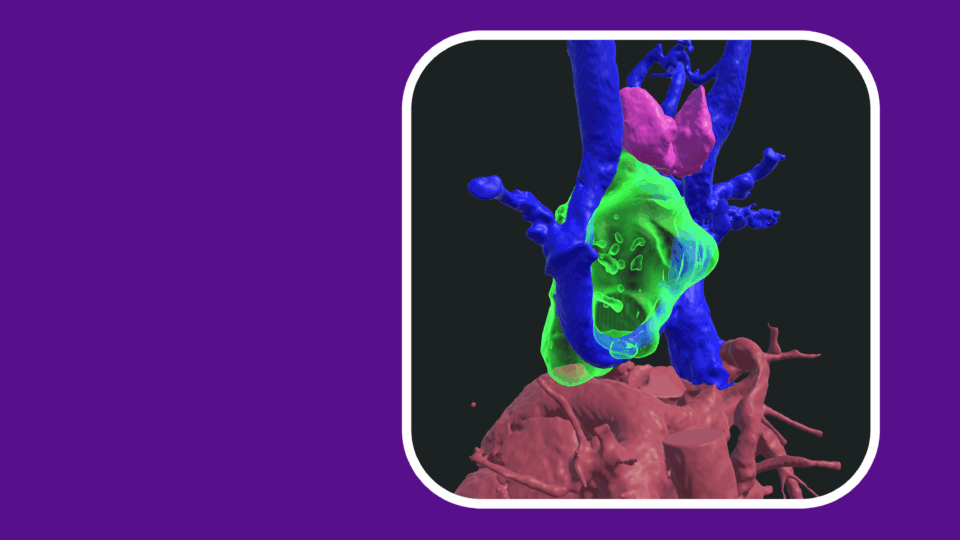
Read a case highlight on Dr. Ovchinsky’s care of a toddler with end-stage liver disease secondary to Alagille syndrome who underwent a split liver transplant.
Physician Focus: Looking ahead, which initiatives are most important for further improving outcomes and expanding access to pediatric liver transplantation?
Dr. Ovchinsky: Our next goal is to develop a comprehensive extracorporeal program for children with acute and chronic liver failure. This program will help stabilize critically ill patients and bridge them to transplant, and in some cases may allow the liver time to recover without the need for transplantation. Establishing this capacity requires specialized teams, advanced training, and sophisticated technology, and would place us among a small number of pediatric programs nationally able to offer this level of care.
“Our next goal is to a build a strong extracorporeal program for children with acute and chronic liver failure.”
We’re also focused on the transition from pediatric to adult care, a period when long-term outcomes, including graft survival, are at greater risk. Dr. Vittorio, the medical director of our pediatric liver transplant program and a national expert in care transitions, is leading a comprehensive program that begins in early adolescence and integrates psychology, social work, and pediatric and adult transplant teams to support patients and families through this critical stage.
We’re also looking ahead to advances in xenotransplantation that may expand future treatment options. As surgical director, Dr. Griesemer brings exceptional expertise to our program in this area.