Referral Notes:
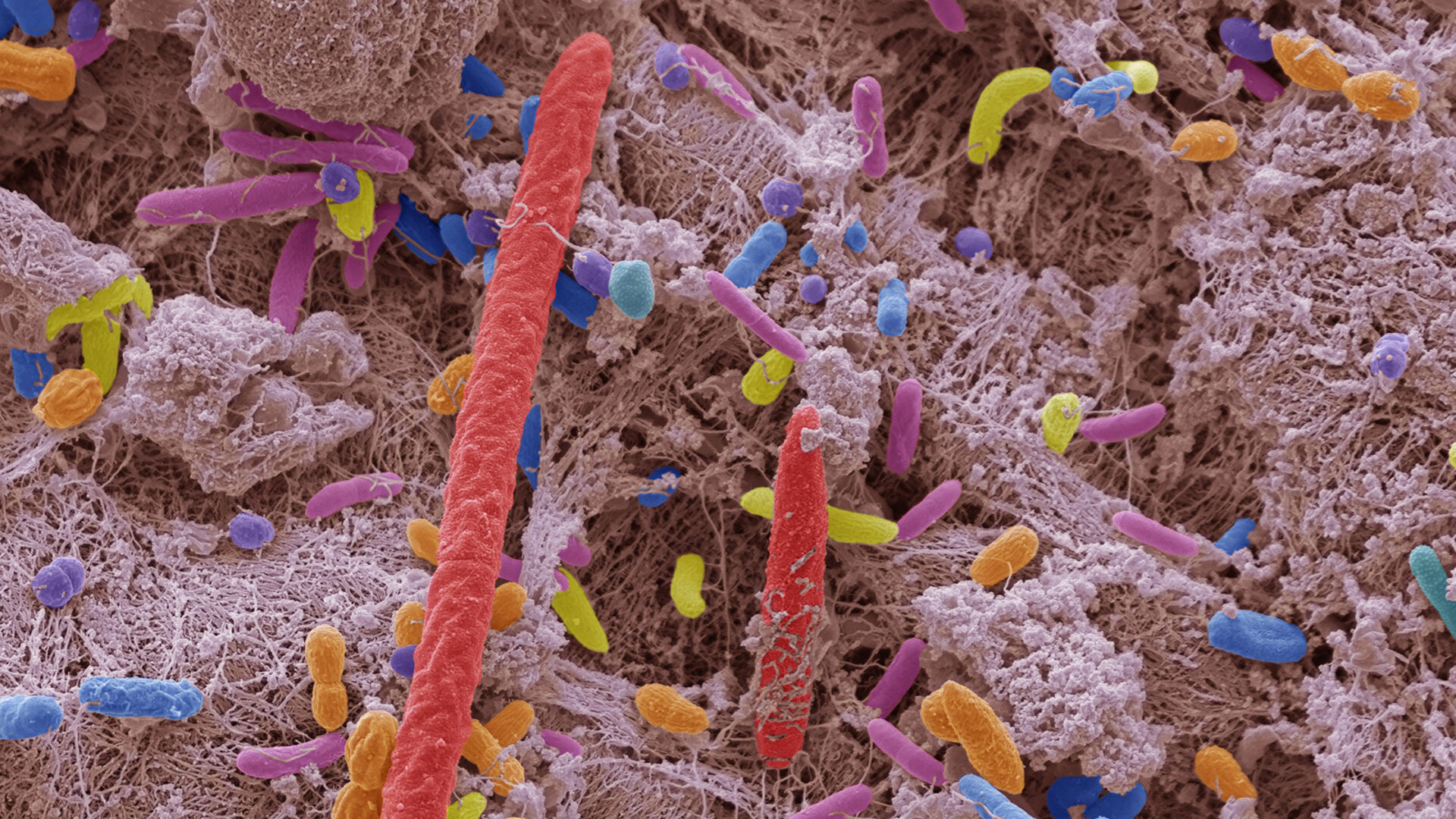
- Analysis of oral samples from two large U.S. cohorts linked multiple bacteria and fungi to higher pancreatic cancer risk.
- A total of 890 participants and matched controls were included in the study, with oral samples collected before cancer diagnosis.
- A Microbial Risk Score based on 27 bacterial and fungal species was linked to a nearly 3.5-fold higher risk of pancreatic cancer.
- The study highlights the oral microbiome as a potential biomarker and preventive target, while noting that causation has not been established.
In the largest and most detailed analysis of its kind to date, researchers from NYU Langone Health and Perlmutter Cancer Center identify 27 species of oral bacteria and fungi that are collectively tied to a nearly 3.5 times greater risk of developing pancreatic cancer. The findings, published in JAMA Oncology in September 2025, add to growing evidence linking the oral microbiome to pancreatic carcinogenesis.
“The oral microbiome may serve as an easily accessible biomarker of pancreatic cancer risk, and potentially as a target for preventive interventions.”
Tamas A. Gonda, MD
“The oral microbiome may serve as an easily accessible biomarker of pancreatic cancer risk, and potentially as a target for preventive interventions,” says study co-author Tamas A. Gonda, MD, co-director of NYU Langone’s Pancreatic Disease Program.
Study Design
The study drew on data from two large U.S. cohorts: the American Cancer Society Cancer Prevention Study-II cohort and the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial cohort. The ongoing, prospective studies are following participants nationwide to examine how diet, lifestyle, medical history, and other factors may influence cancer risk.
Across both cohorts, oral samples were available for 122,000 participants. Among these individuals, 445 developed pancreatic cancer and were matched with 445 cancer-free controls.
All oral samples were collected prior to pancreatic cancer diagnosis. “This allows rigorous assessment of the microbe–disease temporal relationship, as the prediagnostic microbiome is not influenced by the cancer,” wrote the authors.
Key Findings
Analysis revealed several known periodontal disease pathogens—including Porphyromonas gingivalis, Eubacterium nodatum, and Parvimonas micra—as being associated with increased odds of pancreatic cancer. Additional risk-associated taxa included multiple species within the phyla Actinobacteria and Bacteroidetes, a species of Fusobacterium, and several Fermicutes.
“By profiling bacterial and fungal populations in the mouth, oncologists may be able to flag those most in need of pancreatic cancer screening.”
Jiyoung Ahn, PhD
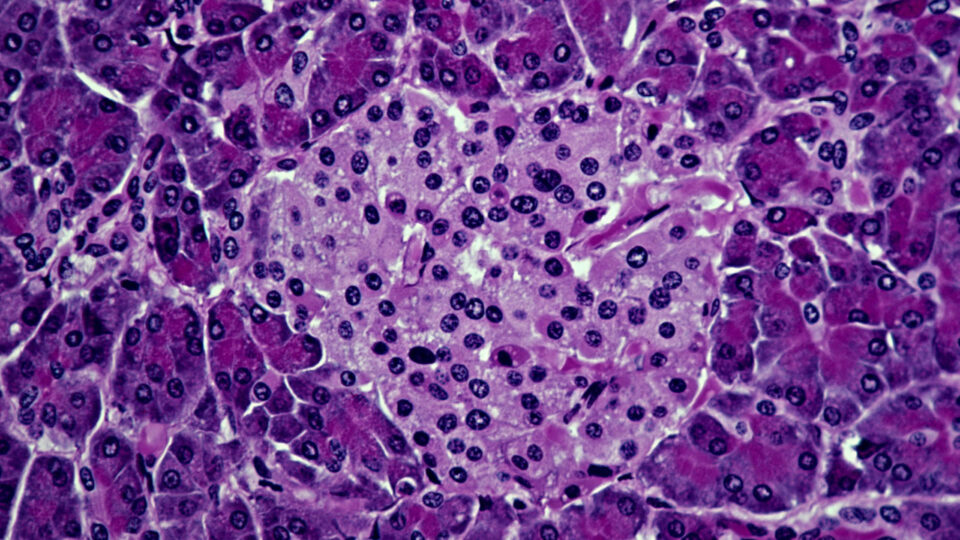
Among oral fungi, the genus Candida was associated with an increased risk of pancreatic cancer. The authors note that, to their knowledge, this is the first study of its kind to suggest a potential role for oral Candida in pancreatic cancer development. Notably, the same Candida species were also detected in patients’ pancreatic tumor tissue.
The researchers then used 27 of the risk-associated bacterial and fungal taxa to create a Microbial Risk Score (MRS), with a higher score representing a higher likelihood of pancreatic cancer. Specifically, for every 1-standard deviation increase in MRS, the odds of pancreatic cancer were 3.44 times higher.
“By profiling bacterial and fungal populations in the mouth, oncologists may be able to flag those most in need of pancreatic cancer screening,” says study co-senior author and population health expert Jiyoung Ahn, PhD, associate center director for population science at Perlmutter Cancer Center.
Next Steps
The authors emphasize that the study was designed to identify correlations, not to establish a causal relationship between oral microbes and pancreatic cancer. Further investigation will be required to determine whether these microbes play a direct role in tumor development.
Next, the team plans to investigate whether oral viruses could contribute to cancer risk and how the oral microbiome may influence pancreatic cancer survival.
“Our findings add to others documenting the far-reaching role of the oral microbiome on overall health,” says Dr. Gonda.