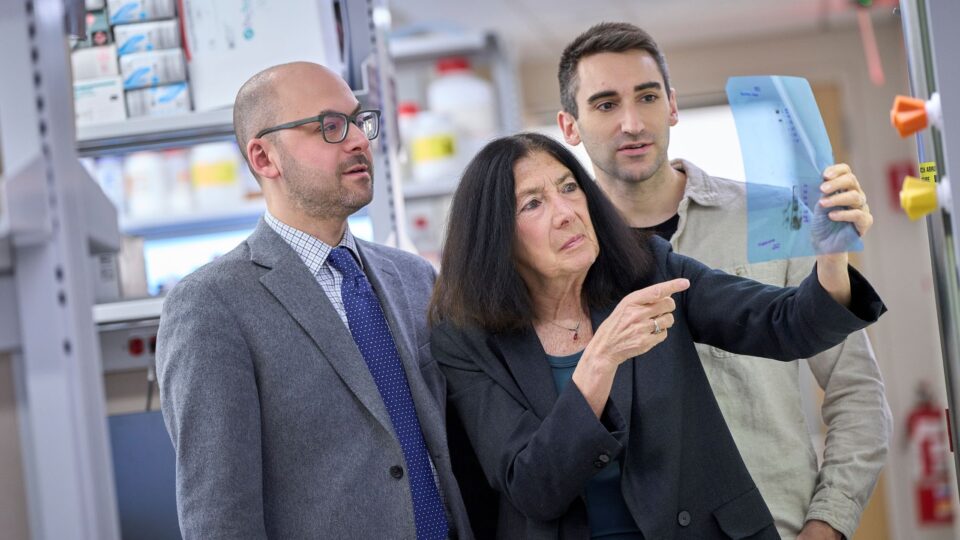
Internationally distinguished surgeon-scientist Jose L. Peiro Ibanez, MD, PhD has joined Hassenfeld Children’s Hospital as director of the newly established NYU Langone Advanced Fetal Care Center.
Throughout his career, Dr. Peiro has developed many novel techniques in fetoscopic surgery and performed basic research to better understand congenital malformations such as spina bifida, gastroschisis, and congenital diaphragmatic hernia. At NYU Langone, Dr. Peiro will develop a comprehensive fetal surgery program and continue his extensive research to advance methods for correcting congenital malformations in utero, focusing on providing the best possible outcomes for infants and their families and maximizing patients’ quality of life.
Previously, Dr. Peiro served as director of endoscopic fetal surgery at the Cincinnati Children’s Fetal Care Center at Cincinnati Children’s Hospital Medical Center. He is recognized for performing the first laparotomy-assisted fetoscopic spina bifida repair in Europe, and the first ex utero intrapartum (EXIT) procedure in Spain.
Here, he discusses his career journey from Barcelona to New York City, his vision for the new center, and his research advancing fetal surgery.
Physician Focus: Can you tell us a little about yourself and what inspired you to join NYU Langone?
Dr. Peiro: In Barcelona where I’m from, I started as surgeon and dedicated time to babies and newborns. I realized the malformations we were treating began as an initial prenatal diagnosis. An observership in fetal surgery at Children’s Hospital of Philadelphia brought me to the U.S. in 2001, when there were very few programs like it at the time. From that early training, I was captivated by the idea that we could intervene in fetal life to change a child’s future.
“From that early training, I was captivated by the idea that we could intervene in fetal life to change a child’s future.”
Jose L. Peiro, MD, PhD
I took what I learned back to Barcelona in 2002 and for the next 11 years, I led a fetal surgery program at Vall d’Hebron University Hospital, incorporating innovative techniques and translational research from the lab to generate new strategies for minimally invasive fetal surgery. I performed Europe’s first laparotomy-assisted fetoscopic spina bifida repair and Spain’s first EXIT procedure to secure the airway at delivery.
In 2013, I was recruited to Cincinnati Children’s Hospital as director of endoscopic fetal surgery. During my tenure there, we incorporated new techniques and participated in many clinical trials.
Leaving Cincinnati was a big decision, but I was drawn to the exciting opportunity at NYU Langone to expand an advanced fetal surgery program and build on NYU Langone’s foundation of caring for complex prenatal diagnoses to better serve patients so they don’t have to travel outside the area for specialized fetal and neonatal surgery. The center will combine expertise in surgery, maternal–fetal medicine, genetics, and diagnostics with multidisciplinary pediatric teams.
Physician Focus: What are your top goals as director of the Advanced Fetal Care Center?
Dr. Peiro: My first goal for the next three to five years is to build on a comprehensive program for diagnosing and delivering the full range of fetal interventions for congenital malformations, with referrals from maternal–fetal medicine across and outside the health system.
I also want to reinforce our research efforts to discover and test new treatments and innovative devices, while fostering collaboration with other centers. I’m the chair of innovation for the North American Fetal Therapy Network, which encompasses about 40 centers. It provides a strong framework for collaboration and creating multicenter clinical trials, which is central to advancing in utero endoscopic fetal procedures.
Physician Focus: Of your current research projects, which are you most excited about right now?
Dr. Peiro: I have four patents, one of which is on synthetic amniotic fluid. It’s designed to replace saline or lactated Ringer’s solution during fetal surgery. The formulation we created with Braxton Forde, MD, and Marc Oria, PhD, at the University of Cincinnati better emulates natural amniotic fluid, preserving up to 90 percent of the amniocytes in the amniotic membranes. Our product will hopefully reduce the risk of prematurity after fetal surgical interventions.
Another exciting project focuses on surgical intervention of fetal hydrocephalus, where we are studying how to recirculate and bypass the obstructed cerebral aqueduct to reduce brain compression and allow better fetal brain development. We have a lot of data in animal models and we’re working to translate this surgery to humans. We’re also exploring an innovative treatment for repairing gastroschisis in utero.
“It’s incredibly rewarding to see how these minimally invasive fetal surgeries can make a lifetime of difference.”
Physician Focus: What’s one of the most common in utero surgeries you perform?
Dr. Peiro: By far, the most frequent intervention is fetoscopic laser surgery for monochorionic twins with twin-to-twin transfusion syndrome, which affects 20 percent of twin pregnancies. In Cincinnati, we did three to four cases per week. In the past 12 years, I’ve had more than 1500 cases. More centers are offering this surgery because the condition is so frequent, but it’s still not widely available. In a metropolitan area like New York City, there’s a major opportunity to provide this specialized surgery to meet the needs of more patients close to home.
It’s incredibly rewarding to see how procedures like fetoscopic laser surgery can make a lifetime of difference, and I’m honored to join NYU Langone and work with a team dedicated to supporting families from diagnosis through delivery and beyond.