Referral Notes:
-
Nearly half of patients with MS use cannabis to treat symptoms, leading to increased risk of cannabis use disorder (CUD).
-
Existing therapies for CUD are limited in both efficacy and accessibility.
- An NYU Langone-led study tested a novel, home-based approach for CUD in patients with MS—remotely supervised transcranial direct current stimulation (tDCS).
- Patients treated with tDCS showed significant improvements in withdrawal symptoms, cannabis use, and MS symptoms, suggesting a safe and effective new therapy.
More than 40 percent of people living with multiple sclerosis (MS) use cannabis to treat their symptoms. Although the psychoactive substance can help control pain and spasticity, potential side effects include cognitive impairment, mood problems, and in some cases, psychosis. In addition, approximately 30 percent of users develop cannabis use disorder (CUD), characterized by an inability to curtail excessive consumption that interferes with normal activities and relationships.
No FDA-approved treatments exist for CUD, and though various behavioral and psychotherapies are available, their efficacy and accessibility are limited. In a pilot study recently published in Drug and Alcohol Dependence, a team led by NYU Langone Health researchers investigated a novel, home-based approach for treating the disorder in patients with MS—remotely supervised transcranial direct current stimulation (tDCS) paired with mindfulness meditation.
“This intervention could potentially be useful for addressing cannabis addiction in other populations as well.”
Leigh E. Charvet, PhD
“Our findings suggest that tDCS can be a safe and effective method for treating CUD in patients with MS,” says senior author Leigh E. Charvet, PhD, who directs the tDCS Program at NYU Langone. “We believe this intervention could potentially be useful for addressing cannabis addiction in other populations as well.” Giuseppina Pilloni, PhD, a research assistant professor in the Department of Neurology, served as first author.
An Emerging Therapy With Broad Applications
Since its introduction in the early 2000s, tDCS has emerged as a promising therapy for a broad range of neurologic and neuropsychiatric disorders. Although some uses of the technology have been approved in the European Union and elsewhere, it remains investigational in the United States.
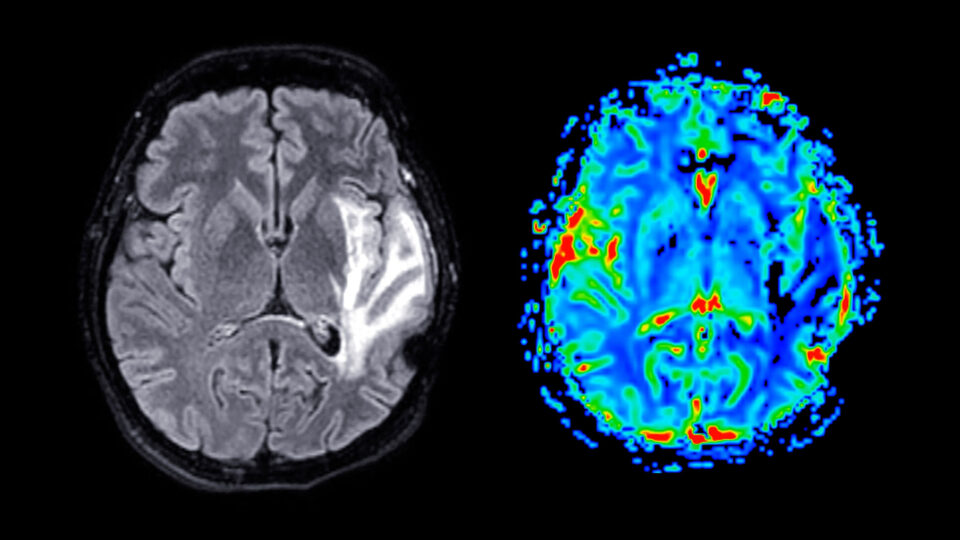
The technique is typically used to optimize outcomes of cognitive and motor exercise programs through functional targeting, in which current is directed to the brain region engaged in a training activity. Imaging studies suggest it works by increasing blood flow in those areas and enhancing neuroplasticity.
Unlike other noninvasive brain stimulation technologies, such as transcranial magnetic stimulation (TMS), tDCS is suitable for home-based delivery, improving access for patients who are unable or unwilling to travel to a clinic for treatment. In this model, sessions are conducted remotely under one-to-one supervision by a technician.
Dr. Charvet has pioneered research on remotely supervised tDCS for more than a decade. After finding that the method boosted the effects of a brain-training program in treating cognitive impairments in patients with MS, she and her team achieved similar outcomes in patients with conditions ranging from depression and post-traumatic headache to post-acute sequelae of COVID, and in those with cognitive, motor, or language impairments resulting from traumatic brain injury, stroke, Parkinson’s disease, and other neurodegenerative conditions.
In 2019, under her direction, NYU Langone established the nation’s first tDCS telehealth program, which has since treated hundreds of patients nationwide.
The new study grew out of Dr. Charvet’s clinical work with patients with MS, who often find it difficult to cut back on cannabis use despite its undesirable complications.
“Many of our patients come to us saying they’re not thinking clearly, and some are experiencing mood and cognitive changes that may be related to heavy cannabis use. But they’re stuck in a cycle of dependence.”
“Many of our patients come to us saying they’re not thinking clearly, and some are experiencing mood and cognitive changes that may be related to heavy cannabis use,” she says. “But they’re stuck in a cycle of dependence.”
Targeting the Neural Circuitry of Addiction
To break that cycle, Dr. Charvet and her team paired tDCS with guided mindfulness meditation, which is often used in treating substance use disorders (SUDs) to reduce cravings and stabilize mood and cognitive states. Stimulation was directed at the dorsolateral prefrontal cortex (DLPFC), which plays a key role in regulating emotional distress and executive function—and, a growing body of evidence suggests, in the neural circuitry of addiction.
Although a few small studies have shown tDCS to be promising in treating SUDs, this was the first to test a remotely supervised version of the technique for that purpose. The team recruited 52 women with relapsing-remitting MS (the most common form of the disease) and CUD. Each participant was provided with a preprogrammed headset and accessories, as well as a laptop for live supervision.
The double-blinded study was principally designed to test feasibility and preliminary efficacy. Participants were randomized in a 2:1 ratio to receive either active or sham tDCS, both paired with mindfulness meditation. The intervention consisted of 20 daily half-hour sessions over four weeks.
“Our main objective was proof of principle,” says Dr. Charvet. “We wanted to lay the foundation for larger studies.”
Results Suggest Potential for Other Populations
The results were positive across virtually all metrics. A robust 83 percent of participants completed the trial, and none dropped out due to adverse events.
In the active cohort, withdrawal symptoms were reduced by an average of 27 percent, compared to 7 percent in the sham group. Frequency of cannabis use also decreased significantly in the active group, while remaining unchanged in those who received sham treatment. MS-related symptoms and cognitive performance improved in the active group as well, with no significant changes in the sham cohort.
Encouraged by these findings, Dr. Charvet and colleagues plan to expand their study of this intervention in MS and have launched an NIH-funded clinical trial to test whether the same approach can benefit individuals with CUD in the general population.
“As cannabis becomes ever more widely available, there’s an exponentially growing need for therapies to help people who become dependent on it,” she says. “We’re excited to see if this technique can contribute to meeting that need.”