A woman in her 30s with neurofibromatosis type 2 (NF2) and bilateral vestibular schwannomas was referred to Danielle Eytan, MD, facial plastic and reconstructive surgeon at NYU Langone Health, for specialized care. She experienced right-sided facial paralysis with minimal functional improvement after undergoing translabyrinthine resection of a right acoustic neuroma in January 2024.
The patient’s extensive surgical history—which involved the removal of 13 tumors along her spine, wrists, and most recently in her brain—complicated the case.
Prior to her surgery in January, she had no paralysis. Although bevacizumab was started after the procedure to shrink the contralateral tumor, it did not respond, suggesting she may require a second surgery. Facial electromyography (EMG) studies at the six-month follow-up revealed only small improvement in tone around the mouth and eyebrow. Additionally, the patient continued to experience intermittent eye dryness and incomplete closure of the right eye.
At that time, Dr. Eytan discussed right-sided masseteric nerve transfer with partial hypoglossal nerve transfer and eyelid weight as a potential surgical intervention to reinnervate her facial muscles. For advanced cases like this one, Dr. Eytan employs a nuanced approach, enabling varying levels of control over facial segments and resulting in improved functional outcomes.
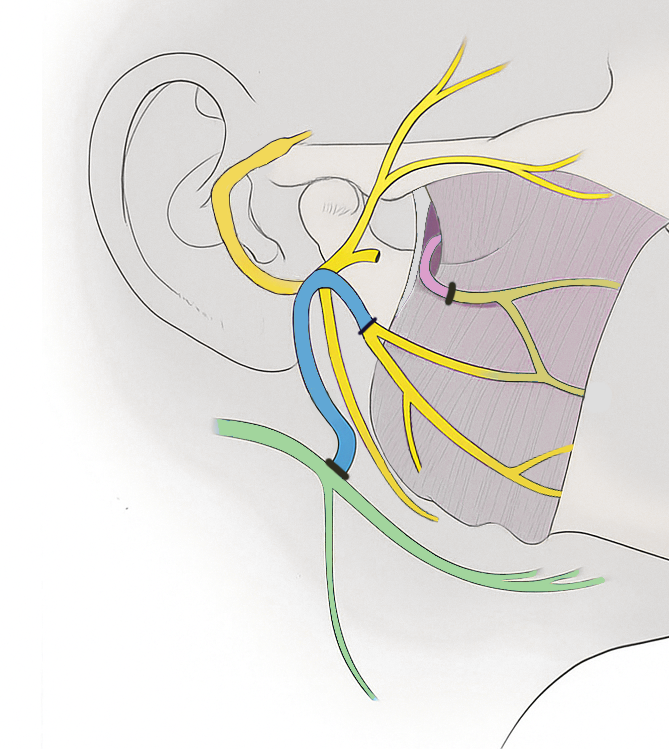
According to Dr. Eytan, the dual nerve transfer technique has shown positive results in cases of complete and partial facial paralysis—many of which have been managed by her and the multidisciplinary team at the Comprehensive Neurofibromatosis Center, led by J. Thomas Roland Jr., MD, professor of otolaryngology—head and neck surgery, and John G. Golfinos, MD, chair of the Department of Neurosurgery.
“With NF2, multiple tumors often result in a complex clinical picture including partial or complete facial paralysis,” Dr. Eytan says. “Following neuroma resection, if there is no recovery of facial movement within six months, masseteric or hypoglossal nerve transfer might be warranted to reinnervate the facial muscles before atrophy occurs.”
“If there is no recovery of facial movement within six months, masseteric or hypoglossal nerve transfer might be warranted.”
Danielle Eytan, MD
The team performed the procedure in August 2024, and it was a success, restoring the patient’s smile and greatly improving her function. Her quality of life returned far sooner than would have been expected, and she even competed in the New York City Marathon just two months after the procedure.
“On the morning of the marathon, her smile came back for the first time,” Dr. Eytan says.
In the months that followed, the patient continued with intensive facial physical therapy at Rusk Rehabilitation to further enhance her recovery.