Referral Notes:
- Early lab studies from NYU Langone found that treating neurons with the ADT drug abiraterone led to reduced brain-derived neurotrophic factor (BDNF) levels and impaired mitochondrial function—hallmarks of compromised neuronal health.
- A forthcoming clinical trial will combine exosome analysis, cognitive testing, and brain imaging to uncover targets for preserving cognitive function during long-term testosterone suppression.
Ongoing research from NYU Langone Health aims to help inform treatment protocols for patients with advanced, recurrent prostate cancer who experience cognitive side effects from testosterone-inhibiting medications.
After initial preclinical research demonstrated a connection between androgen deprivation therapy (ADT) and molecular hallmarks of compromised neuronal health, a clinical trial is in development to further isolate the molecular effects of these medications in men undergoing prostate cancer treatment. In doing so, the researchers hope to identify therapeutic targets that counteract the impact of ADT on cognition.
“We want to deliver the cancer-fighting benefits of these medications without the limitations of their cognitive side effects,” says study senior author Aaron E. Katz, MD, chair of the Department of Urology at NYU Grossman Long Island School of Medicine.
Containing Cancer—with a Cognitive Cost
Cognitive impairment—including memory loss and fatigue—is a well-documented side effect of declining testosterone and is associated with a range of causes, including aging and certain medications. For men with refractory, late-stage prostate cancer, brain fog is a persistent side effect of long-term treatment, observed in up to half of patients on ADT.
“Fortunately, these drugs can effectively keep patients in remission; unfortunately, they come with a significant cost to cognitive function,” says Dr. Katz.
“We want to deliver the cancer-fighting benefits of these medications without the limitations of their cognitive side effects.”
Aaron E. Katz, MD
Cognitive issues associated with treatment can be so severe they lead to poor treatment adherence and discontinuation of therapy. Yet, research into mitigating these effects is an area of unmet need. Although previous studies have demonstrated the return of cognitive function once testosterone is replaced, it remains unclear how to mitigate brain fog when testosterone must be suppressed long-term.
To that end, Dr. Katz is collaborating with Long Island colleagues Allison B. Reiss, MD, an associate professor in the Department of Medicine, and Aaron Pinkhasov, MD, chair of the Department of Psychiatry, to better characterize the connection between testosterone deprivation and cognitive function. In addition to their ongoing research, the team published a literature review analyzing the current understanding of ADT and its associated cognitive deficits.
Isolating Cellular Impacts of Low Testosterone
In initial cell culture studies, the team introduced the drug abiraterone to a neural cell line exposed to androgen to observe molecular changes that may be associated with cognitive decline. Preliminary analysis revealed two key changes in abiraterone-treated neurons compared to untreated neurons: reduced expression of brain-derived neurotrophic factor (BDNF), a protein associated with nerve function and survival, and reduced expression of genes associated with healthy mitochondrial function, including mitochondrial transcription factor A (TFAM).
“These types of changes are well documented in the context of several neurologic disorders.”
Allison B. Reiss, MD
“These types of changes are well documented in the context of several neurologic disorders,” explains Dr. Reiss, a molecular biologist whose research includes neuronal loss in Alzheimer’s disease. “Both BDNF reduction and mitochondrial suppression are biomarkers for compromised neuronal health and poor brain plasticity.”
Based on this existing understanding of these dynamics and their impact on cognitive health, the team is now developing a clinical trial to explore how these and other molecular changes might play out in patients on hormone therapy for prostate cancer.
Finding a Target to Protect Cognition
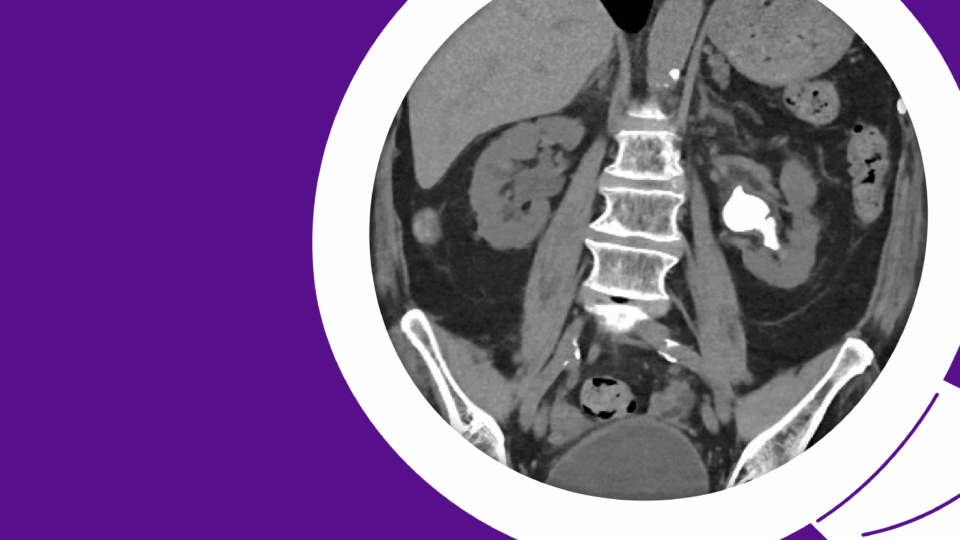
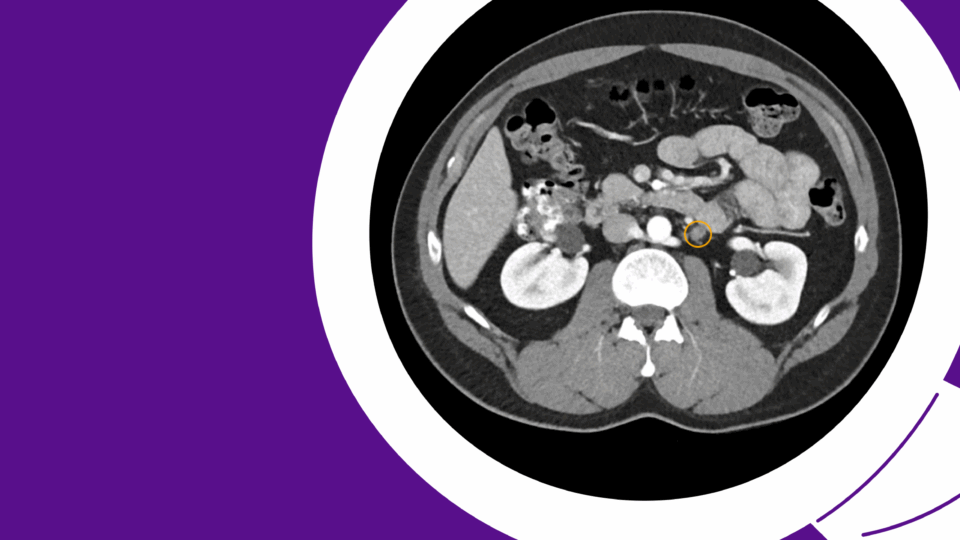
In the forthcoming trial, patients will provide blood samples before and after initiation of ADT. Using immunocapture, members of Dr. Reiss’s lab will isolate brain-derived exosomes from the blood samples for analysis. Because brain tissue cannot be sampled from these patients, the exosomes serve as a proxy for their cells of origin.
“These exosomes, which pass through the blood-brain barrier, serve as a microcosm of brain cell chemistry,” explains Dr. Reiss.
Within the exosomes, Dr. Reiss and her team will focus on microRNAs—key regulators of gene expression—to identify changes associated with the initiation of abiraterone. When notable changes are observed, those microRNAs will be isolated and tested on cultured human neurons to determine whether they affect BDNF expression and/or mitochondrial health and energy generation. “This way, we can observe what is going on in actual patients with prostate cancer undergoing testosterone-inhibiting treatment,” adds Dr. Reiss.
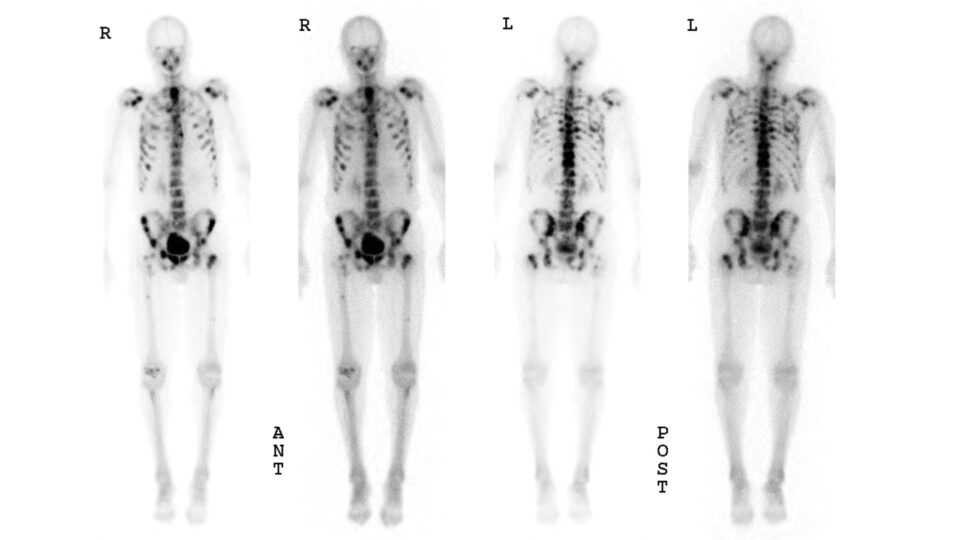
In parallel, Dr. Pinkhasov will perform cognitive testing on the same patients to assess changes in mental function, and brain MRI imaging to document any structural changes in the brain associated with prostate cancer treatment.
By identifying gene expression patterns linked to reduced BDNF or poor mitochondrial health, the team hopes to identify potential therapeutic targets that can be modulated to limit the cognitive decline associated with testosterone suppression.
“Our hope is to isolate and treat the root cause of hormone-associated brain fog for patients with advanced prostate cancer,” says Dr. Katz.