Case Highlights:
- With the tumor located in the lateral ventricles, a right frontal craniotomy provided the safest approach to minimize damage to important structures.
- Neuronavigation, intraoperative MRI, tubular retractors, and ultrasonic aspiration enabled safe removal of 99 percent of tumor tissue.
- Postoperative management included shunt placement for compartmentilized hydrocephalus, with ongoing MRI surveillance for residual tumor growth.
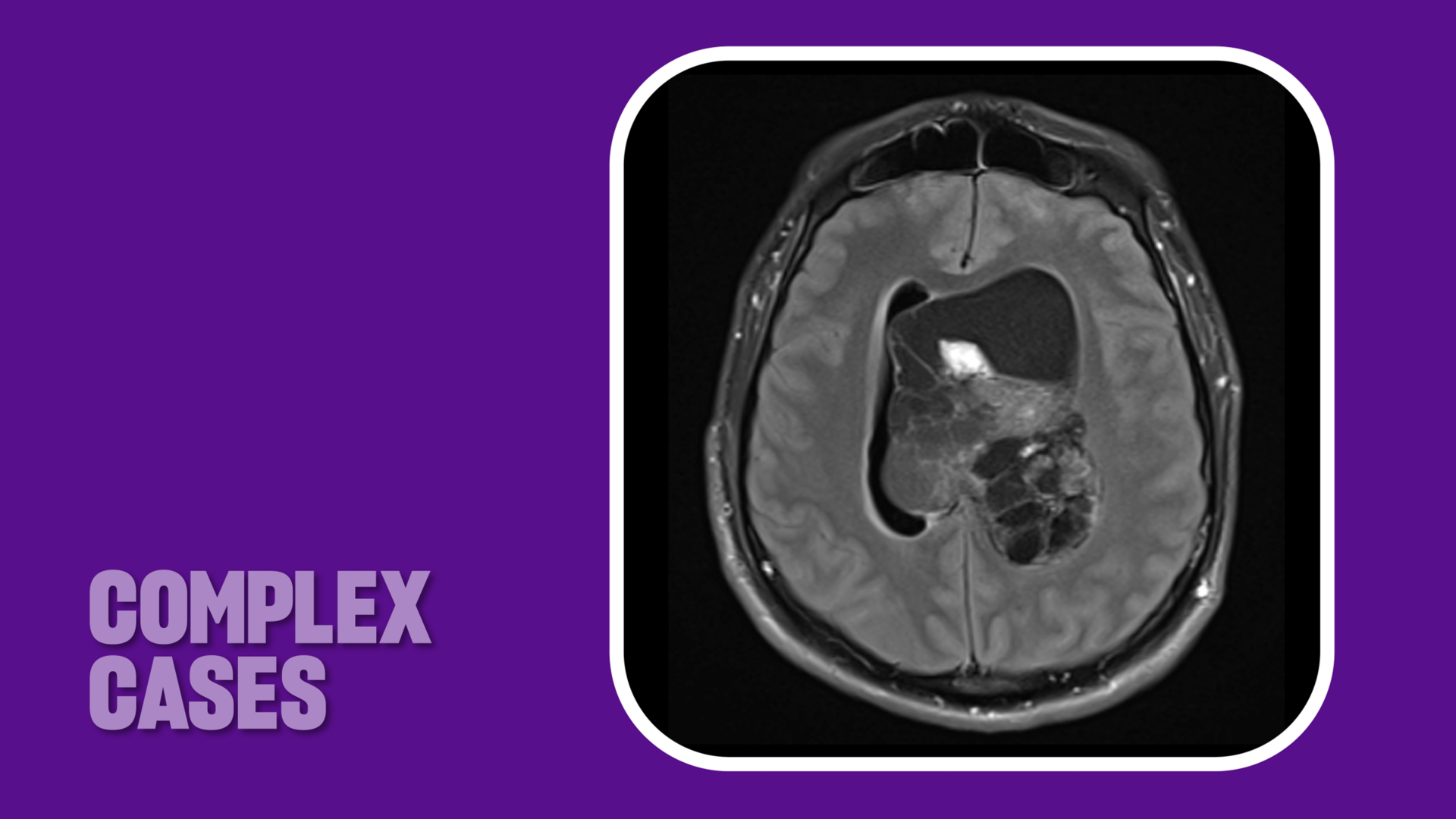
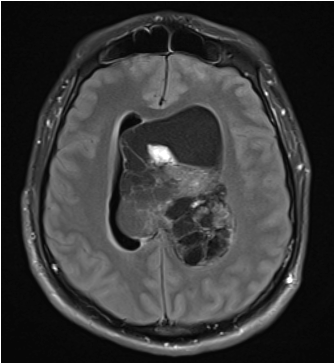
Last fall, a 31-year-old male was diagnosed with a large central neurocytoma at a New Jersey hospital and emergently transferred to NYU Langone Health’s Tisch Hospital for definitive management. Due to the intraventricular tumor’s size and location, the patient was experiencing life-threatening symptoms related to hydrocephalus, including headache, nausea, vomiting, double visible, as well as pressure waves causing a transient loss of consciousness.
“The tumor was so large that it was blocking the circulation and reabsorption of cerebrospinal fluid,” says neurosurgeon Dimitris G. Placantonakis, MD, PhD, attending physician on the case.
After the patient was intubated and magnetic resonance imaging (MRI) performed to inform neuronavigation, the patient was immediately taken to surgery where Dr. Placantonakis and colleagues successfully resected 99 percent of the grade II tumor. “At 110 cubic centimeters, it was the largest intraventricular tumor I had ever encountered,” he says.
Complex Craniotomy Expertise
With the tumor positioned deep inside the brain in the lateral ventricles, Dr. Placantonakis performed a craniotomy using a right frontal approach, which offered the safest advantage for sparing superficial tissue. Making an 8-centimeter linear incision behind the patient’s hairline, he inserted a cannula into a sulcus to create a portal for tubular retractors. Neuronavigation helped guide the team’s approach into the ventricular system to the tumor target.
“At 110 cubic centimeters, it was the largest intraventricular tumor I had ever encountered.”
Dimitris G. Placantonakis, MD, PhD
Resecting the tumor required a combination of standard surgical techniques for central neurocytoma resection, tailored to the tumor’s size and location within the ventricular system, including coagulation, aspiration, ultrasonic aspiration, and physical removal with tumor forceps.
“We were cautious to not violate the walls of the ventricular system because of underlying white matter tracts, and to avoid injury to the fornices and large veins within the ventricular system,” Dr. Placantonakis says. “Intraoperative MRI provided real-time information on how much of the tumor we had resected and areas of residual tumor we could still access.”
The team resected the vast majority of the tumor, leaving only small areas on the ventricular wall. These were deemed unsafe to resect due to the risk of injuring corticospinal fibers controlling movement of the contralateral leg and arm. The hemorrhagic nature of the tumor contributed to the surgical complexity.
During surgery, the tumor was biopsied and sent to NYU Langone’s neuropathology lab for histological and genomic analysis, which confirmed the tumor as a grade II central neurocytoma. DNA methylation profiling of the tissue further supported the diagnosis of a central neurocytoma. While declined by the patient, NYU Langone also offers advanced technologies to characterize tumor cells and their genomic landscape, including targeted gene sequencing to identify mutations that may inform tumor-specific therapy.
Postoperative Management
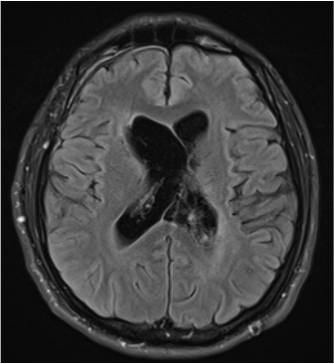
After all excisable tumor tissue was safely removed, Dr. Placantonakis placed an external ventricular drain to address the patient’s ongoing hydrocephalus, now due to blood products rather than tumor. The hydrocephalus eventually became compartmentalized, requiring a revision and placement of two different shunt systems. These shunts will remain in place long term to manage the condition.
The patient will also continue to be monitored with periodic MRIs. “There are small amounts of residual tissue we’re choosing to follow because we’re not sure whether those areas are actually tumor that’s going to grow,” Dr. Placantonakis says. In the event of tumor recurrence, treatment options include additional surgery or radiotherapy.
Meanwhile, after several months of physical and cognitive therapy, the patient made a full recovery. “For a tumor like this, there are so many risks. Cognition, memory, movement, and sensation—all could be at risk along with his life and he’s done spectacularly,” says Dr. Placantonakis. “He’s back to work and fully functional, so we are thrilled.”