Referral Notes:
- A mobile app called Psorcast (available on iOS devices) lets patients capture multiple pictures and digital assessments to track psoriatic disease.
- In a proof-of-concept study led by NYU Langone Health researchers, clinical validity was demonstrated for six digital assessments performed through the app: percent body surface area affected by psoriasis, erythema, induration, scaling, nail psoriasis, and upper extremity impairment.
- The team is continuing work to advance the app and incorporate additional clinical tools, including an assessment of lower extremity involvement.
A new mobile app called Psorcast allows users to capture images and complete digital assessments to track the signs and symptoms of psoriatic disease. The app—developed by researchers at NYU Langone Health, their Psoriasis and Psoriatic Arthritis Clinics Multicenter Advancement Network (PPACMAN) collaborators, and Sage Bionetworks—gives patients and providers greater insight into disease status without requiring an office visit.
In a new proof-of-concept study published in the Journal of Rheumatology, the researchers show that several app-based assessments achieve significant clinical validity when compared to in-person determinations by rheumatologists and dermatologists specializing in psoriatic disease.
“This app can tell us whether a patient is either progressing to arthritis or having a flare of arthritis using completely new measurements for psoriatic disease.”
Jose U. Scher, MD
“This app can tell us whether a patient is either progressing to arthritis or having a flare of arthritis using completely new measurements for psoriatic disease,” says senior study author Jose U. Scher, MD, director of the Psoriatic Arthritis Center.
Up to 30 percent of people with psoriasis will develop psoriatic arthritis, underscoring the need for continual monitoring of indicators of disease progression or flare-ups.
The Power of Selfies
The evaluation of six digital measures and machine learning models, based on data from 104 participants, was co-led by NYU Langone rheumatologist Rebecca H. Haberman, MD, and former principal scientist at Sage Bionetworks in Seattle, Dan Webster, PhD.
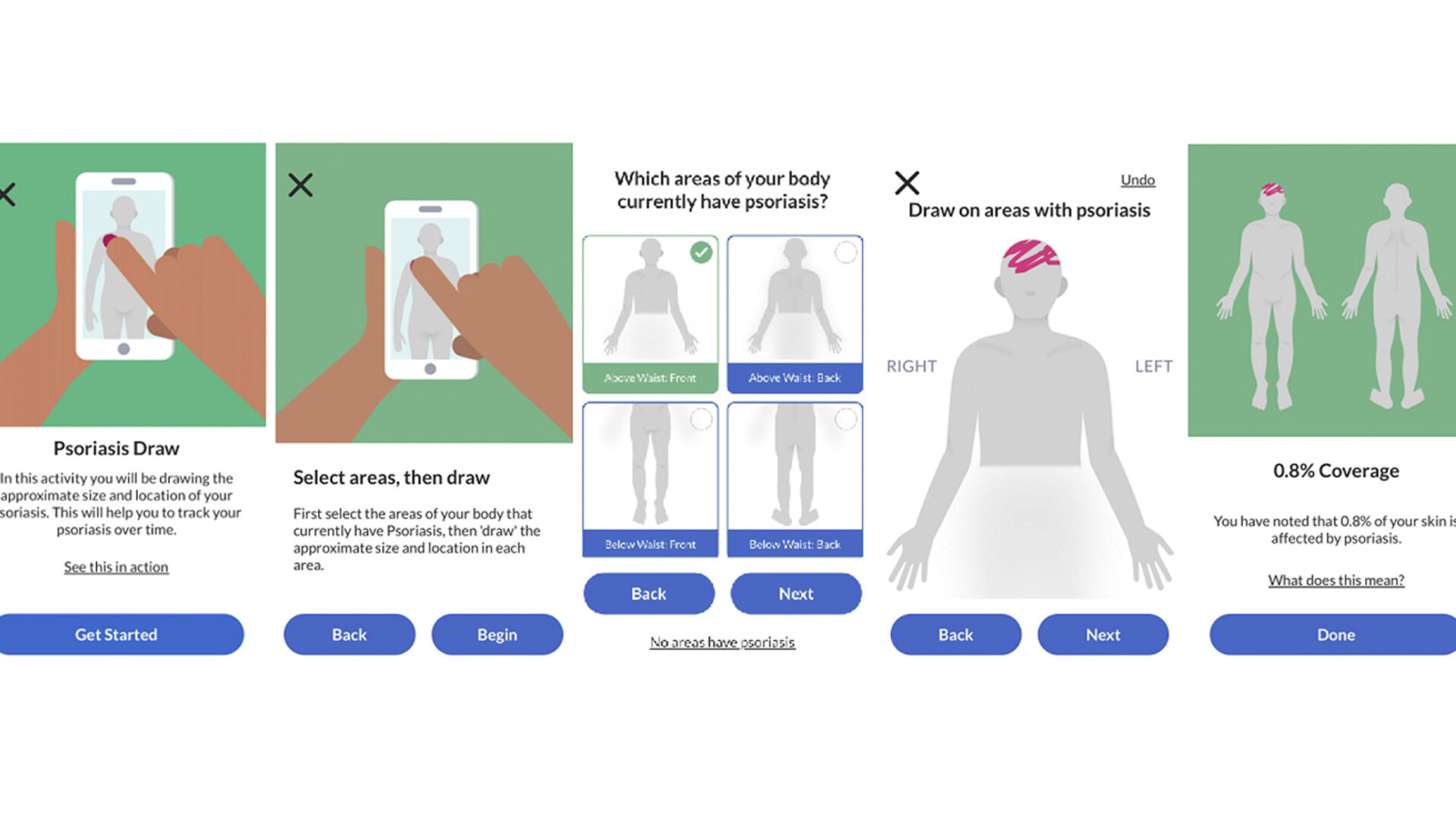
One of the app’s tools, Psoriasis Draw, takes advantage of mobile illustration tools to measure percent body surface area impacted by psoriasis; patients draw on the screen where their skin is affected. In the study, the tool showed a concordance correlation coefficient of 0.94 compared with the physician-assessed body surface area.
“We were able to recapitulate what a doctor would do during a clinical visit to determine the amount of body surface area that’s affected with psoriatic inflammation,” Dr. Scher says.
Other tools within the Psorcast app allow patients to take pictures of psoriatic lesions to track their status over time, including whether and how the lesions respond to treatment. Measurements made by physicians studying the photos matched up fairly well with in-person physical exams, with concordance correlation coefficients of 0.72 for erythema, 0.72 for induration, and 0.60 for scaling.
The app can also capture images of a patient’s hands and feed them into a machine learning model to detect nail psoriasis. When compared to in-person exams, the photo-trained machine learning model identified clinically diagnosed nail psoriasis with an accuracy of 0.76. The results, Dr. Scher says, suggest that the hand images may contain sufficient information for an accurate diagnosis.
Assessing Upper and Lower Extremities
Beyond photos, the team is also using app-collected motion data to aid in assessing psoriasis-related mobility impairments.
The app’s Digital Jar Open tool, for example, evaluates joint tenderness and inflammation in the hand and arm by having patients mimic the movements required to open a jar. “Essentially, we ask people to take their phone and rotate it clockwise and counterclockwise on a table to see how much range of motion the upper extremities have,” Dr. Scher says.
The study found that overall rotation captured by the motion sensor data was significantly decreased in patients with psoriatic arthritis compared to healthy controls or patients with only psoriasis. The overall rotation measure was also sufficient to distinguish patients with and without physician-assessed arm joint tenderness and/or enthesitis.
“Now you’re empowering patients to understand their journey over time. That’s the most important goal if you really think about it.”
One of the app’s newest metrics uses the smartphone’s accelerometer and gyroscope to measure lower extremity flares involving a patient’s ankle or knee via asymmetry of the gait. “That’s because they’re essentially limping,” Dr. Scher says.
While patients walk 30 seconds in a straight line, the Psorcast app counts the steps and symmetry to detect any oscillations. Although the study’s initial test of the measure didn’t show significant discriminatory capacity for confirming lower extremity involvement, Dr. Scher believes a larger cohort size may demonstrate its validity.
The Promise of Self-Monitoring
The results, Dr. Scher says, provide initial evidence of the app’s promise for self-administered monitoring that may further some key goals in disease management. “Number one is, now you’re empowering patients to understand their journey over time. That’s the most important goal if you really think about it,” he says.
Secondly, the app can fill in data gaps between visits to the clinic.
“In a typical clinical trial, you evaluate patients at baseline and again at the end of the study,” Dr. Scher says. But the dynamics between those two points are often unknown. For Phase 2 and 3 trials in particular, he notes, the app can provide important data for clinical comparisons, such as between investigational drug and placebo arms.
Another big benefit of the combined self-administered measurements could be a reduced need for in-person doctor visits—a critical factor given current strains on the healthcare system. Disease activity, in other words, could be closely tracked without the need for constant physician monitoring. “That’s the ultimate goal,” Dr. Scher says.